Researchers identify a target that could combat allergies of early childhood
A pandemic of ailments called the "allergic march" -- the gradual acquisition of overlapping allergic diseases that commonly begins in early childhood -- has frustrated both parents and physicians. For the last three decades, an explosion of eczema, food allergies, hay fever, and asthma have afflicted children in the United States, the European Union, and many other countries.
What causes the march and how to derail it has remained elusive. Now, in this week's Nature, David Artis, PhD, an associate professor of Microbiology at the Perelman School of Medicine at the University of Pennsylvania, and a team of collaborating international scientists, identified that expression of the protein TSLP may influence susceptibility to multiple allergic diseases by regulating the maturation of basophils, an uncommon type of white blood cell. Specifically, TSLP elicits the maturation of a population of distinct basophils that promotes allergic inflammation.
"A fundamental question regarding the allergic march is if a child has eczema, for example, which is associated with TSLP production in skin cells, why would some of those children subsequently be more susceptible to other allergic diseases at different sites of the body such as the gut or the lung?" asks Artis. "Although we have known that TSLP is associated with allergic diseases for many years, how this biological messenger might influence multiple allergic diseases has been a puzzle."
The origins of the present study lie in previous reports that showed that different versions of the gene encoding TSLP, an inflammation-producing cytokine, are associated with increased susceptibility to multiple allergic disorders, and that exaggerated TSLP production is associated with asthma, eczema, and food allergies in children. Together, these studies indicate that TSLP could be a critical regulator of multiple cytokine-associated allergic inflammatory diseases.
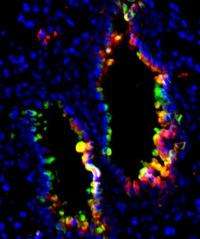
In this new report, mice overexpressing TSLP developed allergic inflammation in their lungs, skin, and gut that was associated with very high levels of basophils. "The critical findings are that TSLP appears to activate the development and maturation of early-stage basophils in the bone marrow and that TSLP elicits a distinct type of basophil," explains first author Mark Siracusa, PhD, a Ruth L. Kirschstein National Research Service Fellow in the Artis lab. Based on these findings, the researchers speculate that this basophil maturation could promote allergic reactions at multiple tissue sites.
To translate these findings to patient populations, Artis and colleagues teamed up with a group of pediatricians at the Children's Hospital of Philadelphia to examine basophil responses in children that suffer from the food allergy-associated disease, eosinophilic esophagitis, which causes inflammation of the esophagus. Previous studies have shown that TSLP is overexpressed in food allergy patients. The team showed in the Nature paper that in children with food allergies basophils exhibited a different molecular make-up compared to non-allergy patients.
"It's promising that after more than 130 years since basophils were first discovered by Paul Ehrlich in Germany, we are still finding out new things about this cell population that could help in the design of new drugs to prevent or better fight allergic diseases," concludes Artis.
With more than 50 percent of Americans estimated to suffer from at least one allergic disease, says Artis, the team is hoping that targeting TSLP and basophils may offer new therapies for multiple allergic diseases.















