Uncovering the spread of deadly cancer
For the first time, scientists can see pathways to stop a deadly brain cancer in its tracks. Researchers at Case Western Reserve University School of Medicine have imaged individual cancer cells and the routes they travel as the tumor spreads.
The researchers used a novel cryo-imaging technique to obtain the unprecedented look at a mouse model of glioblastoma multiforme, a particularly aggressive cancer that has no treatments to stop it from spreading.
A description of their work, and images, will be published Sept. 1 in the journal Cancer Research.
"We're able to see things we couldn't before, and we can use these images to understand how tumor cells invade and disperse," said Susann M. Brady-Kalnay, a professor of molecular biology and microbiology at the Case Western Reserve School of Medicine, and senior author of the paper.
That information, in turn, can be used to help develop and test the effectiveness of drugs and other therapies used to treat the cancer, she said.
To obtain the view, the scientists used a model that included four different cell lines of brain cancers at various stages of tumor development and dispersion. The cancer cells were modified with fluorescent markers and implanted in the model's brain in collaboration with Biomedical Engineering Professor James Basilion's lab.
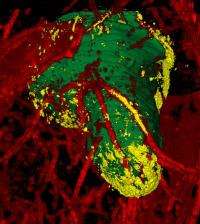
The cryo-imaging system, developed by David Wilson, also a professor of biomedical engineering at Case Western Reserve, disassembles the brain layer by layer and reassembles the model into a color three-dimensional digital image.
Using software and algorithms designed by the researchers, they are able to differentiate the main tumor mass, the blood vessels that feed the cancer and dispersing cells. The imaging system enables them to peer at single cells and see exactly where they are in the brain.
The lead researchers, Susan Burden-Gulley, Mohammed Qutaish and Kristin Sullivant, found that two cell lines, a human brain cancer LN229, and a rodent cancer CNS-1, best resemble the actions of glioblastoma multiforme in human patients.
Reconstructions of models of those two lines enabled the researchers to analyze the extent and patterns of cancer cell migration and dispersal from tumors along blood vessels and white matter tracts within the brain.
The ability to produce such clear and detailed images, the researchers say, will be invaluable when evaluating the potency of drugs and other therapies designed to block dispersal of glioblastoma multiforme cells.















