Neurons grown from skin cells may hold clues to autism

Potential clues to how autism miswires the brain are emerging from a study of a rare, purely genetic form of the disorders that affects fewer than 20 people worldwide. Using cutting-edge "disease-in a-dish" technology, researchers funded by the National Institutes of Health have grown patients' skin cells into neurons to discover what goes wrong in the brain in Timothy Syndrome. Affected children often show symptoms of autism spectrum disorders along with a constellation of physical problems.
Abnormalities included changes in the composition of cells in the cortex, the largest brain structure in humans, and of neurons that secrete two key chemical messengers. Neurons that make long-distance connections between the brain's hemispheres tended to be in short supply.
Most patients with Timothy Syndrome meet diagnostic criteria for an autism spectrum disorder. Yet, unlike most cases of autism, Timothy syndrome is known to be caused by a single genetic mutation.
"Studying the consequences of a single mutation, compared to multiple genes with small effects, vastly simplifies the task of pinpointing causal mechanisms," explained Ricardo Dolmetsch, Ph.D., of Stanford University, a National Institute of Mental Health (NIMH) grantee who led the study. His work was partially funded by a NIH Director's Pioneer Award.
Dolmetsch, and colleagues, report on their findings Nov. 27, 2011 in the journal Nature Medicine.
"Unlike animal research, the cutting-edge technology employed in this study makes it possible to pinpoint molecular defects in a patient's own brain cells," said NIMH Director Thomas R. Insel, M.D. "It also offers a way to screen more rapidly for medications that act on the disordered process."
Prior to the current study, researchers knew that Timothy syndrome is caused by a tiny glitch in the gene that codes for a calcium channel protein in cell membranes. The mutation results in too much calcium entering cells, causing a tell-tale set of abnormalities throughout the body. Proper functioning of the calcium channel is known to be particularly critical for proper heart rhythm – many patients die in childhood of arrhythmias – but its role in brain cells was less well understood.
To learn more, Dolmetsch and colleagues used a new technology called induced pluripotent stem cells (iPSCs). They first converted skin cells from Timothy Syndrome patients into stem cells and then coaxed these to differentiate into neurons.
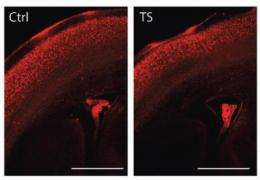
"Remarkable reproducibility" observed across multiple iPSC lines and individuals confirmed that the technique can reveal defects in neuronal differentiation – such as whether cells assume the correct identity as the brain gets wired-up in early development, said the researchers. Compared to those from controls, fewer neurons from Timothy Syndrome patients became neurons of the lower layers of the cortex and more became upper layer neurons. The lower layer cells that remained were more likely to be the kind that project to areas below the cortex. In contrast, there were fewer-than-normal neurons equipped to form a structure, called the corpus callosum, which makes possible communications between the left and right hemispheres.
Many of these defects were also seen in parallel studies of mice with the same genetic mutation found in Timothy syndrome patients. This supports the link between the mutation and the developmental abnormalities.
Several genes previously implicated in autism were among hundreds found to be expressed abnormally in Timothy Syndrome neurons. Excess cellular calcium levels also caused an overproduction of neurons that make key chemical messengers. Timothy Syndrome neurons secreted 3.5 times more norepinephrine and 2.3 times more dopamine than control neurons. Addition of a drug that blocks the calcium channel reversed the abnormalities in cultured neurons, reducing the proportion of catecholamine-secreting cells by 68 percent.
The findings in Timothy Syndrome patient iPSCs follow those in Rett Syndrome, another single gene disorder that often includes autism-like symptoms. About a year ago, Alysson Muotri, Ph.D., and colleagues at University of California, San Diego, reported deficits in the protrusions of neurons, called spines, that help form connections, or synapses. The Dolmetsch team's discovery of earlier (neuronal fate) and later (altered connectivity) defects suggest that disorders on the autism spectrum affect multiple stages in early brain development.
"Most of these abnormalities are consistent with other emerging evidence that ASDs arise from defects in connectivity between cortex areas and show decreased size of the corpus callosum," said Dolmetsch. "Our study reveals how these might be traceable to specific mechanisms set in motion by poor regulation of cellular calcium. It also demonstrates that neurons derived from iPSCs can be used to identify the cellular basis of a neurodevelopmental disorder."
The mechanisms identified in this study may become potential targets for developing new therapies for Timothy Syndrome and may also provide insights into the neural basis of deficits in other forms of autism, said Dolmetsch.
More information: Using iPS cell-derived neurons to uncover cellular phenotypes associated with Timothy Syndrome. Pasca SP, Portmann T, Voineagu I, Yazawa M, Shcheglovitov O, Pasca AM, Cord B, Palmer TD, Chikahisa S, Seiji N, Bernstein JA, Hallmayer J, Geschwind DH, Dolmetsch RE. November 27, 2011. Nature Medicine.


















