Detection, analysis of 'cell dust' may allow diagnosis, monitoring of brain cancer
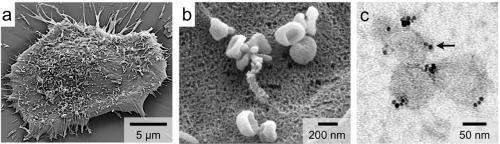
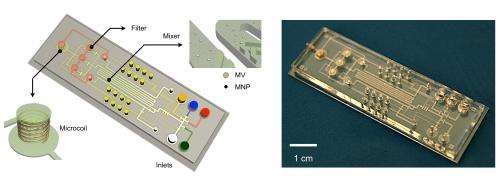
A novel miniature diagnostic platform using nuclear magnetic resonance (NMR) technology is capable of detecting minuscule cell particles known as microvesicles in a drop of blood. Microvesicles shed by cancer cells are even more numerous than those released by normal cells, so detecting them could prove a simple means for diagnosing cancer.
In a study published in Nature Medicine, investigators at the Massachusetts General Hospital (MGH) Center for Systems Biology (CSB) demonstrate that microvesicles shed by brain cancer cells can be reliably detected in human blood through a combination of nanotechnology and their new NMR-based device.
"About 30 or 40 years ago, people noticed something in the bloodstream that they initially thought was some kind of debris or 'cell dust',"explains Hakho Lee, PhD, of the CSB, and co-senior author of the study with Ralph Weissleder, MD, PhD, director of the CSB. "But it has recently become apparent that these vesicles shed by cells actually harbor the same biomarkers as their parent cells."
Circulating tumor cells (CTCs) have been regarded as a potential key to improved cancer diagnosis, but Lee explains, "The problem with CTCs is that they are extremely rare, so finding them in the blood is like trying to find a needle in a haystack." Microvesicles on the other hand are abundant in the circulation and, unlike CTCs, are small enough to cross the blood/brain barrier, which means that they could be used to detect and monitor brain cancers, he adds.
Glioblastoma multiforme (GBM) is the most common and most aggressive brain cancer in humans. By the time it is diagnosed, patients typically have less than 15 months to live. One of the biggest challenges with this condition is accurate disease monitoring to establish whether patients are responding to treatment. Currently, the only way to diagnose and monitor GBM is with biopsies and imaging tests, making long-term treatment monitoring difficult, invasive and impractical. To address this need, the CSB team sought to develop a simple blood test that could be used to easily monitor disease progression.
"The issue with microvesicles, however, is that they are very small, so there are not many technologies out there that can detect and molecularly profile them," explains Lee. "That is where our new technology comes in." By using nanotechnology to magnetically label microvesicles, and by adapting and improving equipment they developed last year to detect cancer cells with a miniature, hand-held NMR, the MGH researchers were able to reliably detect the tumor microvesicles in blood samples from mice bearing human GBM tumors and eventually in samples from human GBM patients.
Compared with other gold-standard techniques, this new technology demonstrated excellent detection accuracy. However, unlike other methods – which can be time-consuming and require much greater sample volumes as well as expertise to perform – NMR detection is quick and simple, potentially providing almost instant results from a small blood sample right in a doctor's office, the authors note. The MGH CSB team is currently extending this platform to other types of cancer and to other diseases such as bacterial infection. A number of clinical studies are currently ongoing, and others are in the planning stages, with the goal of eventually commercializing the technology.
"These microvesicles were found to be remarkably reliable biomarkers," confirms Weissleder. "They are very stable and abundant and appear to be extremely sensitive to treatment effects. In both animals and human patients, we were able to monitor how the number of cancer-related microvesicles in the bloodstream changed with treatment," explains Weissleder. "Even before an appreciable change in tumor size could be seen with imaging, we saw fewer microvesicles. It's like they are a harbinger of treatment response." Weissleder is a professor of Radiology and Lee an assistant professor at Harvard Medical School.
More information: DOI: 10.1038/nm.2994














