Discovery could eventually help diagnose and treat chronic pain
More than 100 million Americans suffer from chronic pain. But treating and studying chronic pain is complex and presents many challenges. Scientists have long searched for a method to objectively measure pain and a new study from Brigham and Women's Hospital advances that effort. The study appears in the January 2013 print edition of the journal Pain.
"While we need to be cautious in the interpretation of our results, this has the potential to be an exciting discovery for anyone who suffers from chronic pain," said Marco Loggia, PhD, the lead author of the study and a researcher in the Pain Management Center at BWH and the Department of Radiology at Massachusetts General Hospital. "We showed that specific brain patterns appear to track the severity of pain reported by patients, and can predict who is more likely to experience a worsening of chronic back pain while performing maneuvers designed to induce pain. If further research shows this metric is reliable, this is a step toward developing an objective scale for measuring pain in humans."
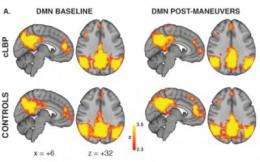
Specifically, researchers studied 16 adults with chronic back pain and 16 adults without pain and used a brain imaging technique called arterial spin labeling to examine patterns of brain connectivity (that is, to examine how different brain regions interact, or "talk to each other"). They found that when a patient moved in a way that increased their back pain, a network of brain regions called Default Mode Network exhibited changes in its connections. Regions within the network (such as the medial prefrontal cortex) became less connected with the rest of the network, whereas regions outside network (such as the insula) became connected with this network. Some of these observations have been noted in previous studies of fibromyalgia patients, which suggests these changes in brain connectivity might reflect a general feature of chronic pain, possibly common to different patient populations.
"This is the first study using arterial spin labeling to show common networking properties of the brain are affected by chronic pain," said study author Ajay Wasan, MD, MSc, Director of the Section of Clinical Pain Research at BWH. "This novel research supports the use of arterial spin labeling as a tool to evaluate how the brain encodes and is affected by clinical pain, and the use of resting default mode network connectivity as a potential neuroimaging biomarker for chronic pain perception."

















