Restrictive Medicaid eligibility criteria associated with higher rates of delayed medical care
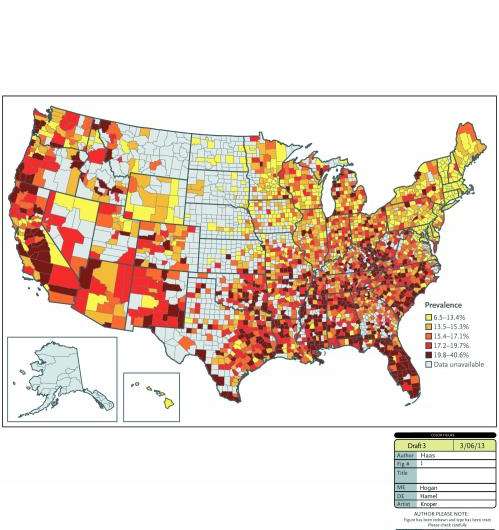
Effective health screening and preventive care is known to reduce health care costs and improve health outcomes, yet new research from Brigham and Women's Hospital (BWH) shows that restrictive Medicaid policies are associated with patients delaying needed medical care due to cost. States and counties with the most restrictive Medicaid eligibility criteria (where individuals must be far below the federal poverty level to qualify for Medicaid) have the highest rates of delayed care.
This research appears in the March 28, 2013 issue of the New England Journal of Medicine.
"The causes of delaying care are complex. States with restrictive Medicaid policies need to review their strategies for improving access to care," said Cheryl Clark, MD, ScD, a co-author of the research and the director of Health Equity Research and Intervention in the Center for Community Health and Health Equity at BWH.
Specifically, the research found:
- States with the most restrictive Medicaid eligibility requirements have higher rates of patients delaying needed medical care.
- Regions with the highest rates of delayed medical care are in the southeast, specifically Florida and Texas.
- Across the United States, Hispanics are at a higher risk for delaying needed medical care.
- Patients are less likely to delay needed medical care in regions with a greater concentration of primary care providers, such as New England.


















