Flu and bacteria: Better prognosis for this potentially fatal combination
Scientists from the Max F. Perutz Laboratories (MFPL) of the University of Vienna and the Medical University of Vienna have provided insights into how much harm bacteria can cause to the lung of people having the flu. An infection with both the flu and bacteria can be a fatal combination. The results could prompt the development of alternative treatments for flu-related bacterial infections, to improve patient outcome and prevent permanent lung damage. The study is published in the renown journal Science.
The flu is caused by an infection with the influenza virus, which mainly attacks the upper respiratory tract – the nose, throat and bronchi and rarely also the lungs. According to the World Health Organization (WHO), around five to 15 percent of the population are affected by upper respiratory tract infections during seasonal flu outbreaks, and between 250 000-500 000 people die of the illness every year. However, a main cause of death in people having the flu is actually a secondary infection with bacteria.
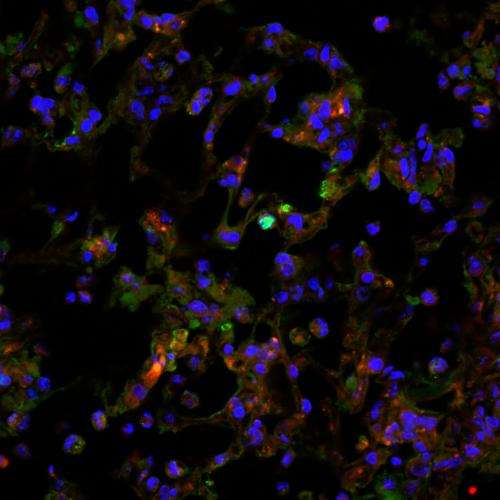
When we are sick with influenza virus, for many reasons our susceptibility to bacterial infection is increased. One type of bacteria that the immune system usually prevents from spreading and becoming harmful for us is called Legionella pneumophila. However in some circumstances, such as when we're infected with influenza virus, Legionella can cause pneumonia, an inflammatory disease of the lung that if left untreated can leave the lung permanently damaged and even cause death. Amanda Jamieson, the lead author of the report and a research fellow in the Department of Microbiology, Immunobiology and Genetics of the University of Vienna, started to study this phenomenon while working in the laboratory of Ruslan Medzhitov, an immunologist at Yale University School of Medicine, USA, and has continued the project in Vienna in collaboration with Dr. Thomas Decker at the MFPL of the University of Vienna and the Medical University of Vienna. "In our model system an infection with influenza and Legionella was fatal. We expected that this would be caused by the bacteria growing and spreading like crazy, but what we actually found was that the number of bacteria didn't change, which was a big surprise", says Amanda Jamieson.
Amanda Jamieson and her collaborators could show now that the damage to the lung tissue caused by a co-infection with flu and Legionella is not properly repaired, as the influenza virus suppresses the body's ability to repair tissue damage. In case of an additional Legionella infection this may lead to fatal pneumonia. However, treatment with drugs that activate tissue repair pathways significantly improved the outcome. This suggests that new treatment options to deal with co-infections of flu and bacteria should be explored. Amanda Jamieson, who will take up an Assistant Professorship at Brown University, USA, in two months, says: "My group will continue to work on tissue repair models and explore different avenues for the treatment of flu/bacterial co-infections."
More information: Amanda M. Jamieson, Lesley Pasman, Shuang Yu, Pia Gamradt, Robert J. Homer, Thomas Decker and Ruslan Medzhitov: Role of tissue protection in lethal respiratory viral-bacterial coinfection. Science (April 2013).














