Lymphatic fluid takes detour
When tumours metastasise, they can block lymphatic vessels, as researchers from ETH Zurich have discovered using a new method. The lymphatic fluid subsequently has to find a new path through the tissue. Such "detours" could well be the reason why metastasis misdiagnoses can occur in hospitals.
A tumour alters the lymphatic system around it – and in a much more complex way than was previously assumed. Tumours are known to release messengers to trigger the formation of new lymphatic vessels. Researchers from ETH Zurich have now discovered that a metastatic tumour can also block lymphatic vessels completely.
The fact that the impact of tumours on the lymphatic system is so diverse underlines the importance of the lymphatic system in cancer and its spreading. Metastases form when cancer cells break away from the original tumour and are washed into a lymph node with the lymphatic fluid, where they can metastasise. As a team of scientists headed by Michael Detmar, a professor at the Institute of Pharmaceutical Sciences, has now revealed, if this metastasis grows it can block the lymphatic flow to the corresponding lymph node. As a result, the lymphatic fluid needs to find a new path through the tissue to another lymph node, effectively taking a "detour".
Nano marker substance for lymphatic tissue
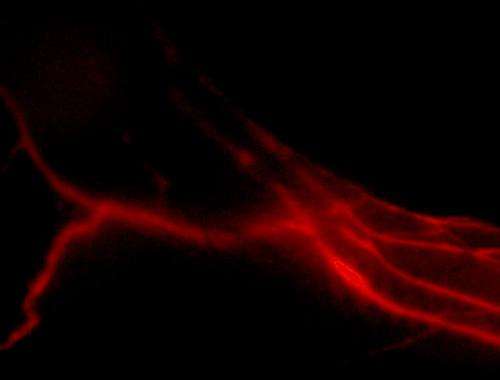
The ETH-Zurich scientists made this observation in experiments on mice using a relatively novel, non-invasive imaging technique called near infrared imaging, which involves injecting a fluorescent substance into the body that "glows" in the shortwave infrared range if stimulated with laser light. Using an infrared camera, the radiation can be recorded and thus the distribution of the marker substance observed. Thanks to one such new substance developed on a nanometer scale by Jean-Christophe Leroux, also a professor at the Institute of Pharmaceutical Sciences, it is now possible to display lymphatic vessels specifically with near infrared imaging for the first time.
To produce the nano marker substance, the researchers combined fluorescent dye molecules with a series of other comparatively large molecules with a precisely defined diameter. In tests conducted on mice, a molecule diameter of eight to ten nanometres proved ideal to render the lymphatic vessels visible. "These molecules are large enough to be transported in the lymphatic fluid yet small enough not to be absorbed by the body's own scavenger cells and transported into the bloodstream," explains Detmar.
Method with benefits
The dye becomes conspicuous by glowing brightly. "We can illuminate anatomical details with it that you couldn't see in the past, such as the tiny lymph valves in the lymphatic vessels," explains Detmar. Because, according to the research to date, the new substance is not toxic and can be excreted back out of the body, it is just the ticket for use in humans in future. Clinical trials are already in the pipeline.
Another advantage over alternative imaging techniques, such as positron emissions tomography (PET): near infrared imaging is much more straightforward. Instead of being reliant on the infrastructure of central hospitals, one day we will be able to use the method anywhere with the aid of portable infrared cameras, even in small medical practices.
Metastases misdiagnoses
According to Detmar, the ETH-Zurich scientists' observation that the lymphatic vessels can be blocked by metastases through to the lymph nodes will have a major impact on cancer medicine. In oncology, the general view is that a tumour that metastasises does so in so-called sentinel lymph nodes, the lymph node into which the lymphatic fluid is conducted from the tumour. In order to detect these sentinel lymph nodes in breast or skin cancer patients, for example, a doctor injects a dye into the tumour. The first lymph node into which this dye is transported is regarded as a sentinel lymph node. During the subsequent biopsy, an expert can determine whether it is a metastatic node.
However, the scientists' work now reveals that this method is not foolproof. After all, if a metastasis in a lymph node blocks the lymphatic flow and the fluid is redirected to another lymph node, as it stands the doctor examines the latter for metastases. If this lymph node is not metastatic, a misdiagnosis can occur, according to which the patient does not have any metastases and thus does not receive the correct treatment. Detmar is convinced that near infrared imaging has a major advantage over conventional methods due to its high resolution: in many cases, the initial stages of the blocked vessels are visible with near infrared imaging.
More information: Proulx, S. et al. Use of a PEG-conjugated bright near-infrared dye for functional imaging of rerouting of tumor lymphatic drainage after sentinel lymph node metastasis. Biomaterials, 2013, 34: 5128-5137. doi: 10.1016/j.biomaterials.2013.03.034
















