Researchers identify key protein's role in cancer development
Researchers at the University of Cincinnati (UC) have identified a key protein as the first dual-function co-regulator of an estrogen receptor that plays a crucial role in cancer development, opening the way to improved therapeutic targets for several types of cancer such as breast, prostate, lung and brain cancer.
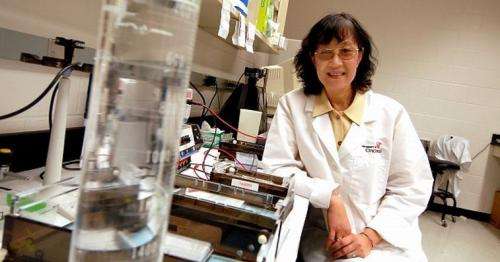
The research was led by Shuk-Mei Ho, PhD, Jacob G. Schmidlapp Chair of Environmental Health and Professor at the UC College of Medicine and director of the Cincinnati Cancer Center, a collaborative initiative of UC, UC Health and Cincinnati Children's Hospital Medical Center. It was published online in the Journal of Biological Chemistry and will appear in the print edition of Aug. 30, 2013.
Ho and her team focused on the interactions between estrogen receptor beta (ER?1) and a co-regulator known as Tip60. Co-regulators are proteins that interact with transcription factors, which are proteins that bind to specific DNA sequences. Co-regulators can be co-activators, which activate gene transcription, or co-repressors, which repress gene transcription.
Unlike estrogen receptor alpha, which plays a role in breast cancer initiation and progression, estrogen receptor beta is a potent tumor suppressor. Co-activating estrogen receptor beta would impair cell growth, thereby halting or slowing the development of cancer. Co-repressing estrogen receptor beta would promote cell growth and therefore encourage tumor development.
Using in vitro models, the team found that Tip60 served as both a co-activator and a co-repressor of estrogen receptor beta, depending on the DNA site involved. Specifically, it served as a co-activator at the binding site known as activation protein 1 (AP-1) but a co-repressor at the estrogen response element (ERE) site.
"For suppression of tumor growth—for example, in cancer treatment—the goal would be to bring Tip60 to estrogen receptor beta as a partnership with any genes that contain an AP-1 site," says Ho. "Therefore, we would want to design new drugs or identify natural products that accomplish this."
Ho notes that the drug fulvestrant, commonly used in the treatment of breast cancer, augments co-activation of Tip60 at the AP-1 site. Plant-derived products such as flax seed, soybeans and tofu contain phytoestrogens that also activate Tip60 at the AP-1 site.
Adds Yuet-Kin (Ricky) Leung, PhD, assistant professor of environmental health at UC and second author of the study, "The important thing to do is to figure out how we can actually bring either a repressor to estrogen receptor beta or an activator to it so cell death activity can be increased or decreased." (Promotion of cell growth, as opposed to the impairment of cell growth sought in tumor suppression, would be beneficial in such examples as wound healing or cardiovascular and brain injury repair, Leung notes.)
















