Bootcamp targets gap in radiation oncologist training
For the patient with laryngeal cancer – a cancer of the voice box – radiation therapy can be a lifeline. Alternately, it could be the thing that takes the patient's voice, before the disease takes their life.
This is precisely why radiation oncologists need training when it comes to contouring, a practice that outlines areas doctors must target to treat cancer, as well as healthy areas they need to avoid exposing to high doses of radiation.
Enter a recent course, hosted by members of the Western and London medical communities.
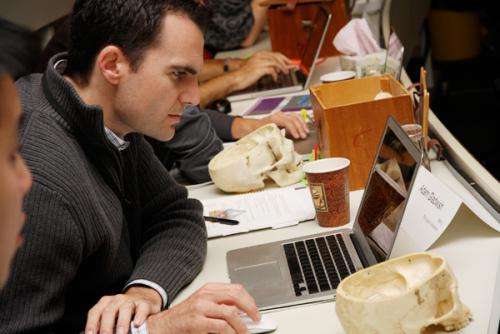
The Anatomy & Radiology Contouring Bootcamp for Radiation Oncology Residents brought together last week 30 residents from medical schools across the country, providing them with an intensive workshop environment to learn anatomy and contouring skills from London Health Sciences Centre (LHSC) doctors and Schulich School of Medicine & Dentistry professors.
"Radiation oncology has changed so much over the past 10 years that the teaching programs have not been able to keep up," said Western Oncology professor Dr. David Palma, a radiation oncologist at LHSC's London Regional Cancer Program.
Palma taught part of the course, and was on the committee that planned the bootcamp. Over the three days, residents worked with imaging scans as well as cadavers to master their skills.
"It used to be designed radiation; we used plain X-rays to design radiation and we'd put squares on X-rays to decide where to treat," Palma said.
However, those days are gone. Today's detailed high-resolution imaging with magnetic resonance imaging (MRI) and computed tomography (CT) scans offer a more detailed look at tumours and healthy tissues.
"Now, with our current ways of giving radiation, we can sculpt our radiation around all types of tumours and all types of normal tissues we want to avoid," Palma continued. "Tumours can be very tricky; they can have almost these tentacles, where they follow different nerves all around the body and it's very important our residents learn to follow where those tumours go, so they can treat them."
A survey across the country revealed radiation oncology residents would jump at the opportunity to take a course such as this. The contouring bootcamp was piloted for the past two years in London; this year was the first time it was offered to residents across the country. With 50 applicants this year, the course was capped at 30 to keep the group small, giving preference to upper-year residents who are closer to taking their exams, Palma explained.
"In radiation oncology, we spend a lot of time trying to figure out what's normal anatomy and what's abnormal anatomy. For the most part, we don't get formalized teaching in that; so it's a lot of learning as you go," said Julianna Caon, a fifth-year resident who attended the bootcamp from the University of British Columbia.
"This was never an area where we felt very comfortable, so when given the opportunity to take this (course), all of the residents in our department wanted to go. The training I got in medical school is not enough," she continued.
"A lot of these things are so intricate, so detailed it's not just easy to learn on your own, or have a natural aptitude for, so the specific training gives you that specific knowledge."
Jonathan Klein, in his fourth year of residency at the University of Toronto, echoed Caon.
"You need to know what's normal and what's abnormal (in anatomy) to give the patient the best chance of cure," Klein said. "If you don't know where the tumour is, the danger is you won't treat all the cancer. If you don't know where it is (and you target healthy tissue), you're going to give the patient undesirable side effects."
Palma said the plan is to continue running the bootcamp, giving other residents the chance to work on their anatomy and contouring skills.


















