New research shows promise for possible HIV cure
Researchers have used radioimmunotherapy (RIT) to destroy remaining human immunodeficiency virus (HIV)-infected cells in the blood samples of patients treated with antiretroviral therapy, offering the promise of a strategy for curing HIV infection. Results of the study were presented today at the annual meeting of the Radiological Society of North America (RSNA).
Highly active antiretroviral therapy (HAART) has transformed the outlook for patients infected with HIV by suppressing the replication of the virus in the body. However, despite the success of HAART in effectively reducing the burden of HIV, scientists believe reservoirs of latently infected cells persist in the body, preventing the possibility of a permanent cure.
"In an HIV patient on HAART, drugs suppress viral replication, which means they keep the number of viral particles in a patient's bloodstream very low. However, HAART cannot kill the HIV-infected cells," said the study's lead author, Ekaterina Dadachova, Ph.D., professor of radiology, microbiology and immunology at Albert Einstein College of Medicine in the Bronx, N.Y. "Any strategy for curing HIV infection must include a method to eliminate viral-infected cells."
In her study, Dr. Dadachova and a team of researchers administered RIT to blood samples from 15 HIV patients treated with HAART at the Einstein-Montefiore Center for AIDS Research.
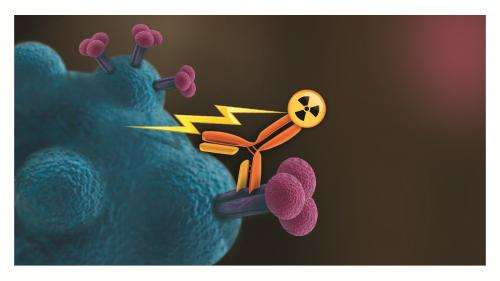
RIT, which has historically been employed to treat cancer, uses monoclonal antibodies—cloned cells that are recruited by the immune system to identify and neutralize antigens. Antigens are foreign objects like bacteria and viruses that stimulate an immune response in the body. The antibody, designed to recognize and bind to a specific cell antigen, is paired with a radioactive isotope. When injected into the patient's bloodstream, the laboratory-developed antibody travels to the target cell where the radiation is then delivered.
"In RIT, the antibodies bind to the infected cells and kill them by radiation," Dr. Dadachova said. "When HAART and RIT are used together, they kill the virus and the infected cells, respectively."
For the study, Dr. Dadachova's team paired the monoclonal antibody (mAb2556) designed to target a protein expressed on the surface of HIV-infected cells with the radionuclide Bismuth-213.
The researchers found that RIT was able to kill HIV-infected lymphocytes previously treated with HAART, reducing the HIV infection in the blood samples to undetectable levels.
"The elimination of HIV-infected cells with RIT was profound and specific," Dr. Dadachova said. "The radionuclide we used delivered radiation only to HIV-infected cells without damaging nearby cells."
An important part of the study tested the ability of the radiolabeled antibody to reach HIV-infected cells in the brain and central nervous system. Using an in vitro human blood brain barrier model, the researchers demonstrated that radiolabeled mAb2556 could cross the blood brain barrier and kill HIV-infected cells without any overt damage to the barrier itself.
"Antiretroviral treatment only partially penetrates the blood brain barrier, which means that even if a patient is free of HIV systemically, the virus is still able to rage on in the brain, causing cognitive disorders and mental decline," Dr. Dadachova said. "Our study showed that RIT is able to kill HIV-infected cells both systemically and within the central nervous system."
According to Dr. Dadachova, clinical trials in HIV patients are the next step for the RIT treatment.


















