July 10, 2014 report
Researchers find interferon has both detrimental and beneficial effects on SIV infected rhesus macaques
(Medical Xpress)—A large team of researchers with affiliations to several facilities in the U.S. and Israel has found that administering Type 1 interferon to rhesus macaques infected with Simian Immunodeficiency Virus (SIV) can have both beneficial and detrimental effects. In their paper published in the journal Nature, the team describes how they found different impacts of interferon on the monkeys depending on when it was administered. Amalio Telenti, of the Institute of Microbiology at the University of Lausanne offers a News & Views piece on this new research in the same journal.
SIV is the simian variety of HIV, which of course is the virus that leads to AIDS in humans. Not long after HIV and AIDS became known in the early 80's, researchers began using interferon as a drug to help prevent HIV from blossoming into AIDS. Interferon is a protein created in the body and released by cells to respond to assumed pathogens such as parasites, bacteria, viruses and even tumors. Adding to the interferon already present, it was hoped would offer even more benefits. Unfortunately, as research continued, little benefit was found when giving interferon to HIV and AIDS patients, causing researchers to look for and find other drugs. In this new effort, the researchers have returned to the idea of using interferon as an HIV therapy by studying its simian counterpart. Thus far, they have found that the results of earlier research didn't take into account when the protein was administered and because of that doctors weren't able to see the beneficial impact the protein could have in inhibiting the progression of the disease.
The researchers actually found two things, the first was that administering interferon to rhesus macaques before they were exposed to SIV helped prevent an infection—doing the opposite by giving them an antagonist of the interferon receptor, led to serious infections. The other thing they found was that timing was important when giving interferon to already infected monkeys.
The researchers found that if they gave the monkeys interferon during the early stages of SIV infection, the protein actually helped slow the infection by slowing the inflammation that occurred as part of the immune system response. But, giving them interferon after the infection was already established appeared to only make things worse. Thus, they conclude, interferon may yet prove to be a valuable therapy for HIV patients, though studies will have to be conducted to determine if it behaves the same way in people, and if it does, if there is a way to determine when the beneficial stage has ended.
More information: Type I interferon responses in rhesus macaques prevent SIV infection and slow disease progression, Nature (2014) DOI: 10.1038/nature13554
Abstract
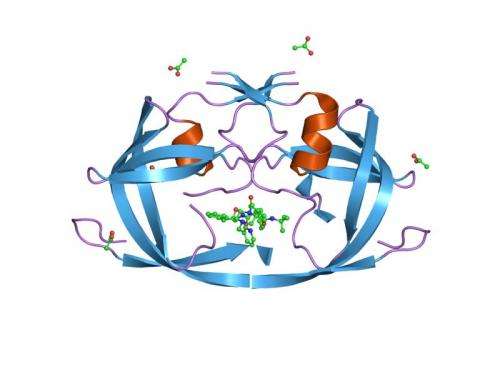
Inflammation in HIV infection is predictive of non-AIDS morbidity and death1, higher set point plasma virus load and virus acquisition; thus, therapeutic agents are in development to reduce its causes and consequences. However, inflammation may simultaneously confer both detrimental and beneficial effects. This dichotomy is particularly applicable to type I interferons (IFN-I) which, while contributing to innate control of infection, also provide target cells for the virus during acute infection, impair CD4 T-cell recovery, and are associated with disease progression. Here we manipulated IFN-I signalling in rhesus macaques (Macaca mulatta) during simian immunodeficiency virus (SIV) transmission and acute infection with two complementary in vivo interventions. We show that blockade of the IFN-I receptor caused reduced antiviral gene expression, increased SIV reservoir size and accelerated CD4 T-cell depletion with progression to AIDS despite decreased T-cell activation. In contrast, IFN-α2a administration initially upregulated expression of antiviral genes and prevented systemic infection. However, continued IFN-α2a treatment induced IFN-I desensitization and decreased antiviral gene expression, enabling infection with increased SIV reservoir size and accelerated CD4 T-cell loss. Thus, the timing of IFN-induced innate responses in acute SIV infection profoundly affects overall disease course and outweighs the detrimental consequences of increased immune activation. Yet, the clinical consequences of manipulation of IFN signalling are difficult to predict in vivo and therapeutic interventions in human studies should be approached with caution.
© 2014 Medical Xpress

















