Obesity and cancer – adding more weight to the evidence

With the nation's ever-expanding waistlines, obesity is never far from the headlines, and you may have seen that today is no exception. A new study – published in the Lancet – has analysed the link between body mass index (BMI) and the risk of 22 of the most common cancer types, and adds further weight to the evidence linking obesity and cancer.
Thanks to years of research, researchers were already pretty sure that seven different types of cancer – including oesophageal, bowel, pancreatic, gallbladder, breast, kidney and womb cancers – were more common among people who are overweight or obese. But the new study – which is of unprecedented size and rigour – brings more types of cancer into the picture
And although we don't fully know why there's a link, these new findings further reinforce the idea that being overweight or obese definitely does increase your risk of cancer.
So what did the new study show?
Weight linked to more cancers than ever before
The researchers, based at the London School of Hygiene & Tropical Medicine, looked at the anonymised medical records of 5.4 million people in the UK, where their GP had recorded their height and weight. This allowed the researchers to calculate each person's BMI – a measurement used to see whether a person's weight differs from what may be expected for their height.
The team then looked at whether a person's BMI meant they were more likely to be diagnosed with cancer during the study.
It's a huge study, and has analysed more data than any previous research. This is important as it gives us really strong evidence about how BMI affects cancer risk.
For the first time, BMI has been linked to 17 specific cancer types, 10 more than previously thought.
But the really interesting findings came when the team looked in detail at how risk changed as BMI increased.
A complex picture
So how did this break down by cancer type?
The results showed that obesity had the biggest effect on a woman's risk of womb cancer – the higher a women's BMI, the higher the chances of subsequently developing the disease.
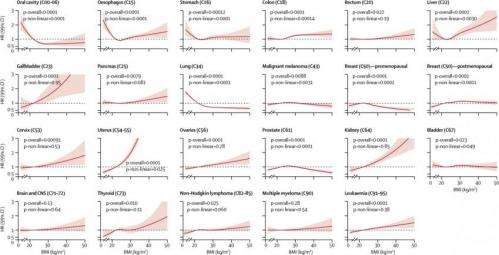
They also found substantial effects on gallbladder, kidney and liver cancers.
And a high BMI was also linked to higher risks of colon, cervical, thyroid, ovarian and post-menopausal breast cancers, as well as leukaemia.
But it wasn't just a high BMI where increased risks were observed. The team also found that being underweight was linked to a higher risk of mouth, stomach and lung cancers – but this could be explained by smoking as the effect disappeared among people who had never smoked, and these are all smoking-linked cancers.
They also found different-sized effects depending on whether you are male or female – being overweight increased the risk of liver cancer more for men than women, for example.
Overall, the team found a 'Goldilocks' effect – some cancers were more common in overweight people, others in those underweight. In other words, the healthiest to be, in terms of cancer risk, is not too large, not too skinny, but 'just right'.
But when the researchers looked at how the risk of different cancers changed in people of increasing BMI, things started to get complicated.
For some tumour types, the risk of cancer increased gradually as BMI increased – a so-called 'linear' relationship. But for others, the risk changed unpredictably as BMI increased.
Ultimately, these results highlight how complicated the links between BMI and cancer are. Such studies will always act as a springboard for more research to understand these risks better, rather than giving a definite answer.
What this study doesn't show
While important and vast in scale, we still don't understand how and why BMI affects cancer risks. There are many theories, but no definite answer – perhaps because, as this study demonstrates, these risks are complicated and don't always follow the same pattern.
To really answer the question, we need studies that get over a few hurdles that the current study didn't address, for example:
Is BMI the best way of measuring obesity? Probably not. While it's the best universal measurement we have it's not clear if BMI is the most accurate way to measure obesity. In fact, a major limitation of this study was the lack of alternative measures for obesity (for example body fat percentage).
What about exercise? Physical activity can reduce the risk of many types of cancer, and wasn't measured either, highlighting another gap in this research.
And perhaps most importantly for working out what advice to give the public, we still don't know whether losing weight will help to lower cancer risk. To find this out, we'll need really detailed data and studies with long follow-up times – but for now, all we can say is that keeping a healthy weight is important.
But despite these limitations the size and statistical robustness of this research makes it the most comprehensive analysis of the obesity/cancer relationship yet.
So what does this all mean for you?
Obesity is an important risk factor for cancer, and this study estimates that 12,000 cases of cancer a year in the UK are due to the nation's weight problem, although previous research has put that number as high as 17,000. This is important, as studies like this can focus people's minds on ways to prevent the disease.
But it's not just about cancer: obesity is a risk factor for many conditions, including diabetes and heart disease. The evidence shows that the detrimental impact of obesity in the UK is mounting, and this study will support the political discussion around obesity at a national level.
It's important to state, though, that research on this isn't about blaming people for their cancer, nor is it about researchers 'telling people what to do'. It's about trying to understand what cancer is, what causes it, and why – so researchers, doctors and policy makers can try to help minimise the terrible burden it places on our society.
And a final point – this new study also shines a light on the importance of anonymised data in medical research. The more data that's made available for research, the more clearly researchers can identify the patterns and reasons for these risks – and ultimately work out how to minimise them.
More information: Bhaskaran K, et al. (2014). Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults, The Lancet, DOI: 10.1016/S0140-6736(14)60892-8

















