Battling drug-resistant pathogens

Evolution kills people. Andrew Read has been saying so for years. But he never actually saw it firsthand until he worked this summer in a hospital in Ann Arbor, Michigan.
That's when Read, who is Evan Pugh Professor of Biology at Penn State, stepped away from his busy University Park lab to study the problem of drug resistance up close, sifting through massive clinical databases and consulting with infectious-disease specialists struggling with difficult cases in real time. He well remembers the first patient he saw die.
"She had a chronic bacterial infection which was unable to be cleared out," he says. "She had been in and out of the hospital for months. The docs who were treating her used one drug after another. When resistance arose, they tried another. Finally, they just ran out of drugs."
Read works in the relatively new field of evolutionary medicine, specializing in infectious diseases. He is best known for his work on malaria, looking for solutions to the rising resistance in humans against antimalarial drugs—and to a similar resistance against insecticides in the mosquitoes that carry the disease.
"Malaria parasites," Read says, "do evolution on steroids. The only way we can stop them evolving in my lab is by freezing them solid." His basic premise is that an overly aggressive, unscientific use of drugs is driving this evolution, and the evolution of many other pathogens.
"We attack these things that harm us—the bugs or the mosquitoes or the viruses or the cancers," he says, "and they evolve back."
Call it adaptation writ large. To a biologist like Read, what's happening is rapid evolution in response to selection pressure—the same force that shaped the bills of Darwin's finches on Galapagos. In this case, he argues, the pressure is being applied by modern medicine.
"That woman in Michigan died of what I think of as uncontrolled evolution," he says. "We don't know how to slow that evolution down."
Adapt or die
The development of antibiotics in the middle of the last century stands among the greatest triumphs of medical science. "In the case of infections," Read says, "these drugs worked just stormingly well. We went from situations where you would die from a prick in the finger to where—surgery, immunosuppression, everything is possible."
Such success has its costs. "People have this expectation that these wonder drugs are going to keep working like that," he continues, "or that there'll be new ones coming along. But new drugs are not coming along at the rate they once did."
One hundred thousand Americans die of infections each year, according to the Centers for Disease Control—at least a quarter of them from drug-resistant infections that were easily cured 20 years ago. And evolution is speeding up: Read says pathogens are now evolving resistance to existing drugs faster than new drugs can make it through the regulatory process.
It's not just antibiotic resistance, either. "The exact same problem applies in cancer," he says. In the United States, where well over half a million people die annually of the disease, "almost all of those are cases where the cancer has evolved resistance to the chemotherapy."
One reason, he says, is the systematic overuse of these drugs, an orthodoxy well-entrenched since Alexander Fleming's discovery of penicillin. The flamethrower approach, Read calls it: full-frontal attack. The clinical object is to wipe out every last trace of infection. The problem, says Read, is that "in evolutionary terms, that very, very strong attack means that the pathogens are under equally strong natural-selection pressure to respond."
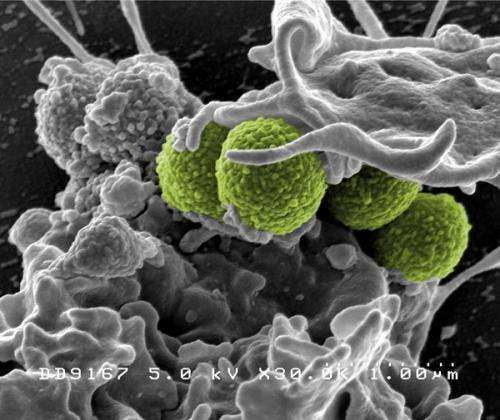
In other words, if you kill all the weak, drug-sensitive bugs, you leave the field wide open for the strong, drug-resistant ones. The least harmful result of this kind of survival of-the-fittest, Read says, is that our drugs grow less and less effective, and eventually fail. The worst case is the development of brand new superbugs, pathogenic strains of extraordinary—and terrifying—virulence.
An emerging perspective in evolutionary medicine, he says, suggests that a different approach may be warranted. "There's an idea that, in cancer treatment for example, maybe you shouldn't be going at it quite as aggressively—you could step back a bit.
"In some mouse experiments," he explains, "better outcomes have been generated by treating a tumor with chemo when it's growing and leaving it alone when it's not growing. A rule like that keeps the tumor there, but also keeps it drug-sensitive. Instead of trying to eradicate the tumor, you go for control."
Read himself has seen similar results—in mice—with malaria parasites. "We set up infections with resistant parasites and sensitive parasites, and we ask, 'What's the best way to treat an infection like that?'" he explains. "Our object is to make the host as healthy as possible as fast as possible. How do you best do that while controlling the resistant strains? And in our hands, with our mice and our strains of parasites, the current guidelines of the World Health Organization—take a full drug course for many days past the time you feel better—is the worst thing you can do. Everything else we've tried works better than that."

Not surprisingly, Read's ideas have caused considerable controversy, especially in medical circles. But after ten years, he says, they are now at least firmly on the scientific agenda. And indeed, he isn't pushing them for clinical use. Not yet. The whole point is that the best course isn't clear.
"Kill every last bug is probably good advice in particular circumstances," he says. "What we don't know is what those circumstances are."
From birds to bugs
As a boy in his native New Zealand, Read dreamed of saving that country's exotic endangered birds. The dream eventually carried him to Oxford University in England, where as a graduate student he began a study of avian blood parasites.
"Toward the end of my Ph.D.," he says, "it dawned on me that nobody was paying much attention to these parasites, even though they are very closely related to malaria parasites which kill people, and they evolve in real time. The field was wide open." The exact same science that had unlocked the secrets of adaptation in Darwin's finches, he realized, could be applied to infectious disease.
There's no one-size-fits-all, he quickly understood. Instead, "We've got to figure out what are the fundamentally important issues, and then ask in any particular disease context, how those fundamental issues apply."
As Read explains, there are two vital components in the evolution of a pathogen: the genetic mutation that is the origin of resistance, and the natural selection that spreads it. "You need both." But depending on the disease, one component can be more important than the other.
In something like HIV, he explains, new mutants are constantly arising, so that resistance pops up all the time. In something like malaria, by contrast, resistance arises extremely rarely—the spread is the issue.
If there is a general rule, it may be this: Treating aggressively is a double-edged sword. It kills bugs so they can't mutate to resistance, but at the same time it amplifies any resistance that might already be present. "These two opposing evolutionary forces will always play out," Read says. "The question is, in each particular case, which will win?"
Vaccines that leak
The same pressures that drive the evolution of drug resistance, Read says, can also play out with vaccines. Think about extremely deadly pathogens —"by which I mean ones that kill everybody all the time," he says.
"There are only a few of these in humans, and they are typically spillover things." So something like the Ebola virus, while it might spill over occasionally to humans from bats or other animal hosts, doesn't circulate widely. The reason is that it kills the host before it spreads, and therefore kills itself. "If you're a bug, you've got to keep the host alive in order to transmit."
With the use of vaccines, however, strains that previously would've been sufficiently nasty to obliterate themselves find themselves in a host who is protected. And if that vaccine is "leaky," i.e., not good enough to prevent transmission, the pathogen can spread to other hosts. "The result is you keep alive in a vaccinated population something that's nastier than what you would've had in the population before." When that strain enters an unvaccinated individual, the results are devastating.
Read believes this is what happened in the case of Marek's disease, a scourge of the modern poultry industry. Sixty years ago, Marek's symptoms in barnyard fowl were mild but in the 1960s the virus became troubling enough in industrial operations to spark development of a vaccine. It became routinely administered to commercially raised chickens. In the decades since, two versions of the vaccine have grown ineffective, with a third showing signs of weakening. Meanwhile, Marek's expression has become lethal. "The strains that are now circulating are so nasty they kill 100 percent of unvaccinated birds within 10 days," Read says.
There could be many contributing factors, he allows, including a half-century's worth of changes in the poultry industry. But "our theoretical work suggests that vaccination alone is sufficient to maintain these hyperpathogenic strains." He is currently conducting experiments to test the theory.
Read emphasizes that Marek's is a leaky vaccine, unlike those that have proved so successful in the eradication of human diseases like measles, mumps, rubella, and polio. But there are several human diseases, he says, including Pertussis, typhus, and human papilloma virus, which may be susceptible to the same possibility.
"One of the concerns I have," he adds, "is that if this theory is correct, then with something like avian flu, where we vaccinate birds to keep them alive, we could be allowing very virulent strains to circulate. To the extent that avian flu is a risk factor for humans, that's a problem."
Sustainable use
When Read speaks about managing the evolution of pathogens, his goals sound deceptively modest. "We might not be able to make things better," he says, "but we should try to avoid making them worse."
That means no more "wasting good drugs" the way we did in the last century. "We need to use them more scientifically," he says. Instead of relying on a constant stream of drug development—engaging in an arms race with nature that we're bound to lose—we need to practice stewardship, finding ways to keep our current drugs effective for as long as possible.
Using drugs thus sustainably, Read acknowledges, "means there's often going to be a trade-off between what we do now for patient health and what might make things safer for the future."
It will also mean trying new things. In the case of HIV, he notes, medical researchers scrambling for a cure figured out that the best approach is combination therapy. "This is an example of where evolution has been tamed," Read says. "And they did it empirically, just by fiddling around with combinations of drugs. My contention is that we can have that sort of success faster if we understand the underlying science."
In the world of agriculture, an evolution-based approach to protecting livestock, he suggests, might include counterintuitive measures like breeding for disease susceptibility instead of resistance—so that infected individuals die off before pathogens are transmitted. "Keeping every chicken alive might be bad," he says.
For slowing the evolution of malaria, conversely, it might be best to let some mosquitoes live. Read and Penn State colleague Matthew Thomas made headlines a few years ago when they developed a fungal insecticide that kills only older mosquitoes. Since only older mosquitoes can transmit the parasite, the theory runs, this is enough to stop the disease from spreading. At the same time, leaving younger mosquitoes alive to breed greatly lessens selection pressure—the reproductive advantage that comes with evolving resistance to the insecticide. With the pressure removed, evolution slows, and the insecticide remains potent much longer.
Mathematical models and laboratory experiments with mosquitoes bear this out, Read says, "but we have had almost no luck getting money to move that project forward.
"It's a big jump from where we are now," he acknowledges, "killing every last mosquito with DDT. I think we might get some traction as resistance to conventional insecticides continues to spread."
In the case of hospital infections, the traction is already there. "All of the physicians I work with are up for anything I've got to say if I've got data to back it up," Read says. "They've got problems, and they want solutions. But they're not going to be persuaded by mouse experiments."
The Michigan patient he saw die, he continues, "had a big effect on me. The doc I was working with said he thought it was a failure of the science. We had uncontrolled evolution and we did not know how to get it under control.
"That's going to be a major challenge in the current century. We need a science that will allow us to make the best and longest use of the drugs we have."



















