Trends of 21-gene recurrence score assay use in older patients with breast cancer
A genetic test for patients with breast cancer that helps to predict the risk of developing metastatic disease and the expected benefits of chemotherapy has been adopted quickly into clinical practice in a study of older patients and it appears to be used consistently within guidelines and equitably across geographic and racial groups, according to a study published online by JAMA Oncology.
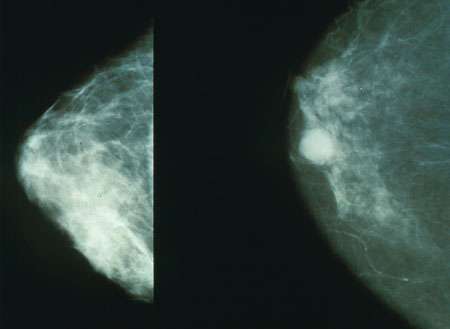
The 21-gene recurrence score (RS) assay was approved for coverage in 2006 by the Centers for Medicare & Medicaid Services. The test is meant for patients with estrogen receptor (ER)-positive, lymph node (LN)-negative breast cancer. The current guidelines recommend using the test to identify patients at low risk of developing metastatic disease who may forgo chemotherapy and patients at high risk for whom the benefits of chemotherapy may be more substantial, according to the study background.
Michaela A. Dinan, Ph.D., of the Duke University School of Medicine, Durham, N.C., and coauthors examined trends in the use of the test among Medicare beneficiaries diagnosed with breast cancer between 2005 and 2009. The authors used patient records from a Surveillance, Epidemiology and End Results (SEER) data set with linked Medicare claims. The study included patients 66 years or older at diagnosis.
The authors identified 70,802 patients and study results indicate use of the test increased from 1.1 percent in 2005 to 10.1 percent in 2009. The majority of the tests (60.9 percent) were performed in patients who met the criteria for National Comprehensive Cancer Network-defined intermediate-risk disease (estrogen receptor-positive, lymph node negative tumors >1cm).
In the overall study population of 70,802 patients, rates of chemotherapy remained similar between 2005 (16.2 percent) and 2009 (15.9 percent). In 18,218 patients with intermediate-risk breast cancer, there was not a statistically significant increase in chemotherapy use between 2005 (8.2 percent) and 2009 (10 percent).
Use of the test was associated with patients who were younger, had fewer co-existing conditions, higher-grade disease and were married. Among patients who were younger than 70 years old with intermediate-risk disease, testing rates increased from 7.7 percent in 2005 to 38.8 percent in 2009, according to the results.
While testing seemed to be modestly higher in the Northeast, the authors found that geographic region was not otherwise associated with testing. There also was no difference in the proportion of black patients among those patients who received the test (5.7 percent) and those who did not (5.9 percent), according to the results.
"Further study is warranted in patients with breast cancer who are not included in the SEER-Medicare database, particularly younger women for whom the factors affecting chemotherapy use and assay use may differ from those observed in our study. Evolving clinical paradigms of clinical management and testing indications, including the use of the assay in node-positive disease, and their impact on costs, chemotherapy use and outcomes at the national level remain important areas of study," the study concludes.
In a related editorial, Lisa Flaum, M.D., and William J. Gradishar, M.D., of the Northwestern University Feinberg School of Medicine, Chicago, write: "Despite the appropriately tested population, the RS score did not result in a significant change in chemotherapy utilization in this older, intermediate-risk group, increasing from 8.2 percent to 10 percent, which was not statistically significant. This contrasts with data demonstrating a more significant change in practice patterns. The lack of change in chemotherapy utilization suggests either that the physicians have a bias about treating older patients with chemotherapy that the test did not change regardless of results, or that the test results were concordant with their pretest bias."
"For the test to have clinical utility in the older population, patients would have to possess an accurate understanding of their risk of recurrence, their life expectancy and a realistic expectation of the toxic effects related to chemotherapy (which many older patients might tolerate well). Physicians have to be willing to recommend chemotherapy to appropriate older patients who have a high RS, patients for whom they might not ordinarily be as definitive in their treatment recommendation as they would be with a younger patient," the editorial notes.
More information:
JAMA Oncol. Published online March 5, 2015. DOI: 10.1001/jamaoncol.2015.43
JAMA Oncol. Published online March 5, 2015. DOI: 10.1001/jamaoncol.2015.32














