Five lessons, and an enduring mystery, from a massive stroke study
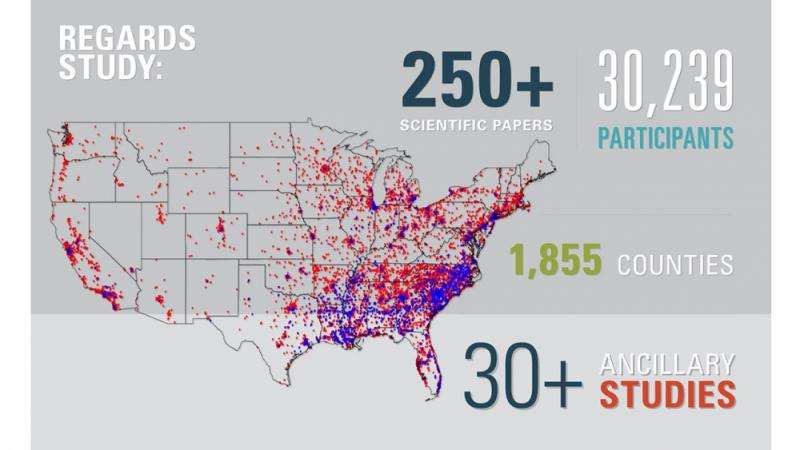
By any measure, the UAB-led REasons for Geographic And Racial Disparities in Stroke (REGARDS) study is a big deal. Funded by major ongoing grants to the School of Public Health (SOPH) from the National Institute of Neurological Disorders and Stroke, REGARDS is the largest population-based study of its kind. Between 2003 and 2007, it enrolled 30,239 participants in 1,855 counties across the United States and continues to follow them to answer two crucial questions: Why do Southerners have a 50 percent higher risk of dying from stroke than the rest of the country? And why are blacks twice as likely to die from stroke as whites?
A traditional epidemiological study to answer these questions, along the lines of the famous Framingham Heart Study, would have required clinics set up across America at a cost of billions of dollars, says George Howard, Dr.P.H., principal investigator of REGARDS and professor in the Department of Biostatistics in the SOPH at UAB. "It would never have been funded, so we decided to break that paradigm."
They did it using the life insurance model. "The trick of REGARDS is we partnered with the people who do life insurance physicals," Howard said. "If you buy a million-dollar life insurance policy, a nurse is going to show up at your doorstep to ensure that you're not getting ready to drop dead." Leveraging those health care professionals to do in-home visits, the REGARDS team collected detailed information from all participants: blood pressure, electrocardiograms, waist circumference and much more, including a blood draw that measured cholesterol, C-reactive protein (a marker of inflammation) and several other factors. The investigators have called participants every six months since, tracking their health changes over time.
That vast flow of information has uncovered important clues to reducing the health burden not only of stroke but also of heart disease, sepsis, kidney disease, fractures and other conditions. "REGARDS is a gold mine for research questions," Howard said. To date, it has generated more than 250 scientific papers and spawned more than 30 ancillary studies. In 2013, UAB signed a memorandum of understanding with the Medical University of Lodz in Poland to explore the possibilities of setting up a similar study across Europe.
A $28 million renewal has funded REGARDS through 2017, and made possible a second round of in-home visits. Data from these visits, collected a decade after the initial visits, will offer crucial insights on the links between risk factors and health outcomes for a wide variety of conditions, from stroke to kidney disease. "We'll be able to look at the change in the risk factors over time and get a better understanding of what it is that is driving these disparities," Howard said.
As REGARDS powers into its second decade, The Mix asked Howard and other investigators to identify some of the study's most significant findings—and lingering questions they are determined to solve.
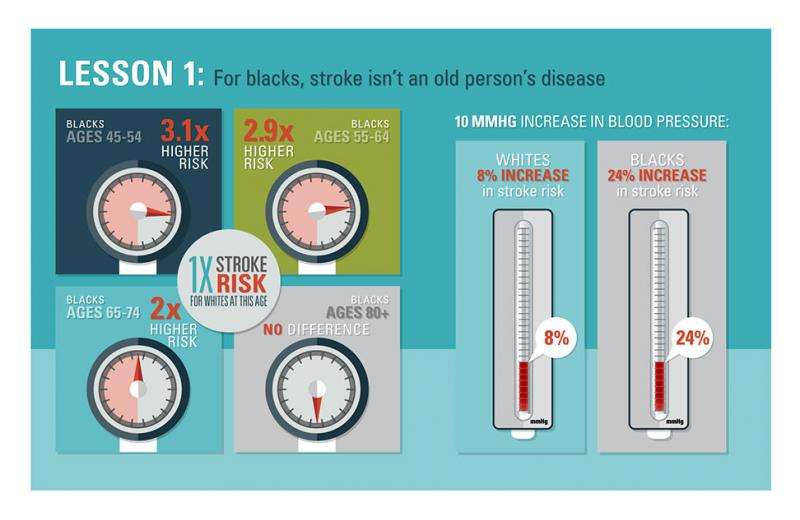
Lesson 1: For blacks, stroke isn't an old person's disease
REGARDS was designed to figure out why stroke disproportionately affects blacks. But what it has shown is that the disparity is largely concentrated among the study's younger age group, Howard says. Among REGARDS participants, blacks ages 45 to 64 are nearly three times more likely to have a stroke than are whites in the same age range. But by the time participants reach their 80s, the disparity has almost completely vanished.
One reason for that massive difference, Howard says, is that high blood pressure, the leading risk factor for stroke, affects blacks more severely than it does whites.
In a 2013 paper in the Archives of Internal Medicine, Howard and colleagues reported that a 10-millimeter increase in blood pressure was associated with a threefold larger increase in stroke risk for blacks compared with whites. "For each 10-millimeter increase in blood pressure, whites have an 8 percent increase in risk; but the same blood pressure increase in blacks is associated with a 24 percent increase" in stroke risk, Howard said. "This difference seems to explain a lot of the additional stroke risk in young black participants."
At prehypertension levels (systolic blood pressures from 120 to 139 mmHg, or diastolic pressures from 80 to 89 mmHg), blacks have a 40 percent higher stroke risk than whites. That rockets up to a 400 percent higher stroke risk for blacks in stage 1 hypertension (systolic pressures from 140 to 159 mmHg and diastolic pressures from 90 to 99 mmHg).
"It really gives a clinician the groups to target to eliminate this disparity," Howard said. Many people think this is a problem of awareness, or access to care, he adds. But REGARDS data show that blacks are significantly more likely to be aware that they have high blood pressure, and to be undergoing treatment, than whites. "It's just that the treatment doesn't work," Howard said. "The real problem is that they are 30 percent less likely to have their blood pressure under control."
Now Howard and colleagues are analyzing REGARDS data to find out which medications are most effective at controlling blood pressure in black participants. "We want to see which works best," Howard said. That information could be invaluable to help physicians improve hypertension control in their patients.
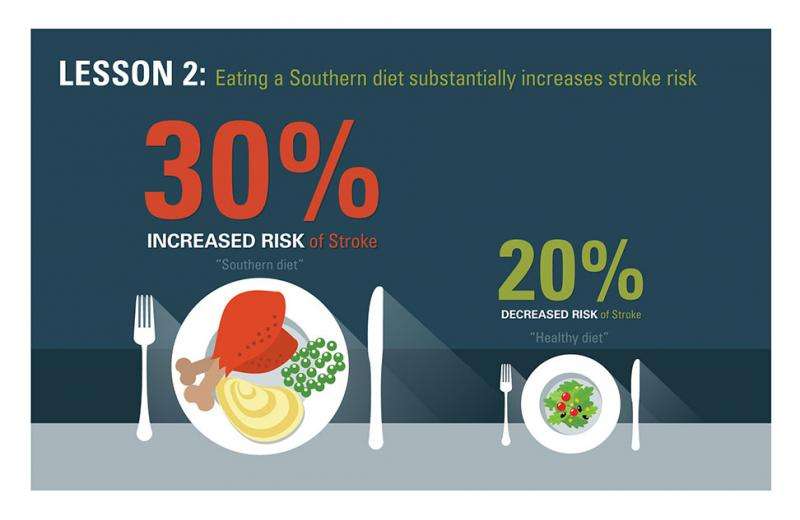
Lesson 2: Eating a Southern diet substantially increases stroke risk
An eight-page, 107-item diet questionnaire filled out by tens of thousands of REGARDS participants has led UAB nutritional epidemiologist Suzanne Judd, Ph.D., to new insights on the link between food and stroke risk.
Judd and colleagues used statistical techniques to find connections in that mass of data points. They uncovered five common dietary patterns, or "foods that people often eat together," she said. The worst in terms of stroke risk was the Southern diet: high in processed meats, fried foods and sugar-sweetened beverages. "We saw a 30 percent increased risk of stroke in people who were eating the Southern diet nearly every day of the week," said Judd, an associate professor in the Department of Biostatistics.
Meanwhile, a "healthy" diet pattern, "with lots of fruits and vegetables, beans, whole grains, lean chicken and lean fish, was associated with a 20 percent reduction in stroke, regardless of race," Judd said. The results were published in the journal Stroke in 2013.
In the new REGARDS cycle, researchers are asking participants about diet again. "Our next question is 'Does dietary change reduce your risk?'" Judd said. "Let's say you ate a Southern diet when we first talked to you and then you switched to a healthier diet: Do you get to assume the risk of the person who eats a healthier diet, or did you retain some negative consequences from your lifetime of eating a Southern diet?"
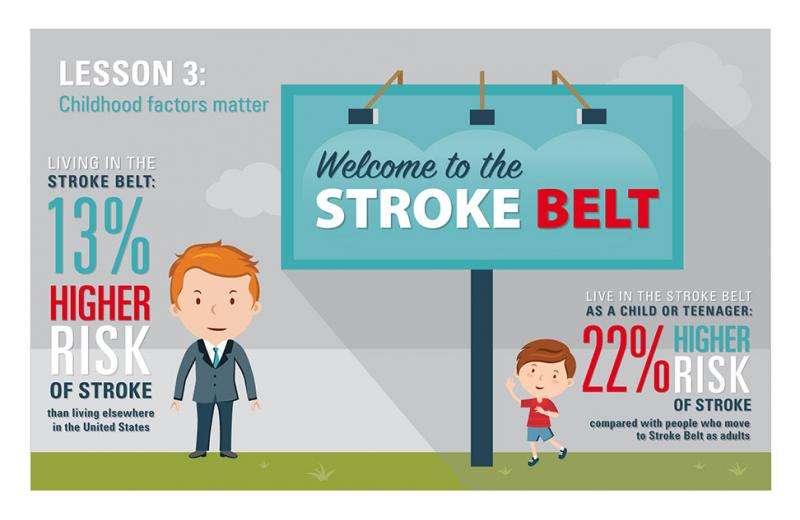
Lesson 3: Childhood factors matter
Living in the Stroke Belt—that is, in Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina, South Carolina or Tennessee—puts you at a 13 percent higher risk for stroke than living elsewhere in the United States. But when you moved to the Stroke Belt also turns out to be important, according to a study published in 2013 in the journal Neurology.
"REGARDS is unique in the sense that we have the entire residential history of our participants," said Virginia Howard, Ph.D., the study's lead author and a professor in the Department of Epidemiology in the SOPH. Analyzing those histories showed that "living in the Stroke Belt as a child or teenager appears to impart about twice as much stroke risk as living there as an adult," she said.
That could be because "the teen years are when you are establishing your habits," Virginia Howard said. "You have a little more control, you're more influenced by your peers, and you can make choices about lifestyle—are you going to exercise or eat fast food, for instance?
"The Stroke Belt is defined by where you die, but we don't know a lot about how you pick up the risk factors over your entire life," Virginia Howard said. This will be a major focus of study for her future REGARDS research, she adds. "We want to show how important early childhood factors are to the rest of your life: the quality of education, where you lived, and the economic and environmental conditions of where you lived as a child. In that way, we can help develop policies and programs that address these issues, and reduce the number of people who go on to have a high risk of stroke later in life."
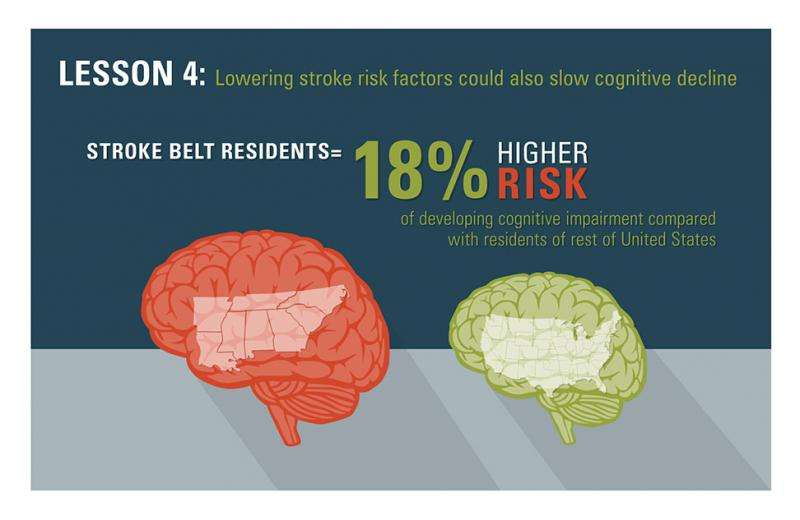
Lesson 4: Lowering stroke-risk factors also could slow your cognitive decline
Quick: How many animals can you name in a minute? Your abilities on that test are a good indication of your executive function, or "the ability to organize one's thoughts to initiate and carry out a task," said Virginia Wadley, Ph.D., a professor in the Department of Medicine and director of the Dementia Care Research Program in the Division of Gerontology, Geriatrics and Palliative Care.
Wadley has analyzed results from thousands of tests like these, carried out over the phone with REGARDS participants, to find out how a person's stroke-risk factors relate to his or her mental functioning. In a 2011 study in the Annals of Neurology, researchers found that "among stroke-free participants, incidence of cognitive impairment is higher here in the Southeastern U.S. Stroke Belt, even after controlling for regional variations in age, race and education," Wadley said. In fact, Stroke Belt residents had an 18 percent higher risk of developing cognitive impairment.
Moreover, the higher one's stroke risk, as measured by the Framingham Stroke Risk Profile scores, the higher the risk of cognitive decline. "So, controlling vascular risk factors like hypertension and diabetes is important for preventing not only stroke but also cognitive decline," Wadley said.
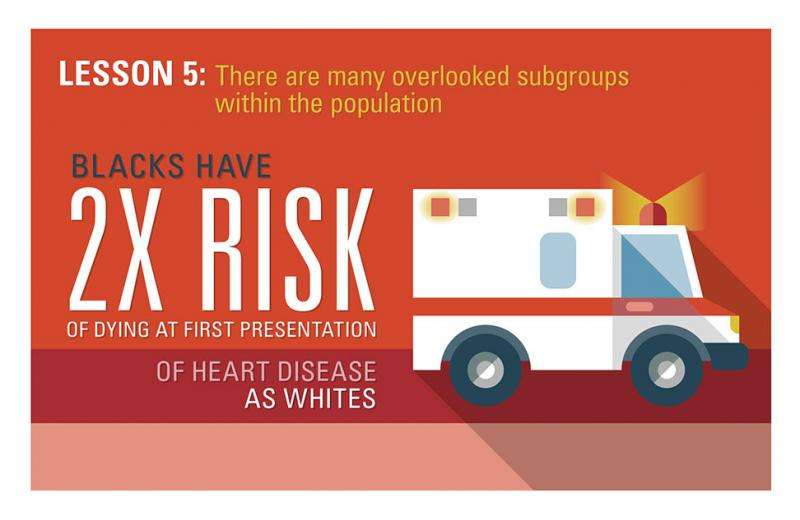
Lesson 5: There are many overlooked subgroups within the population
One of the major contributions of REGARDS is its ability to identify subgroups of individuals who are slipping through the health care cracks, says Monika Safford, M.D., professor in the Division of Preventive Medicine and principal investigator for the REGARDS-MI (Myocardial Infarction) ancillary study.
"REGARDS is a great opportunity to really understand what is going on, not just in stroke but in heart disease and other conditions as well, and to help health care professionals and policy makers focus their attention on where they may be overlooking things," Safford said.
In a 2012 study in the Journal of the American Medical Association (JAMA), Safford and colleagues found that blacks had twice the risk that whites had of dying at their first presentation of heart disease. "And all of that was explained by risk factors," she said. "The way to get that problem under control is to do a better job on cholesterol and smoking and high blood pressure—all things that we know how to do. We described that there was a difference; but we also described why that difference existed—so if we want to fix it, we know exactly what we need to do."
A 2013 study in JAMA, written by Orlando Gutierrez, M.D., associate professor in the Department of Medicine, found that higher levels of a protein in the urine called albumin were associated with a greater risk of heart disease in black individuals than in white individuals. With REGARDS, "we're looking marker by marker at potential differences that deserve more attention in blacks versus whites," Safford said.
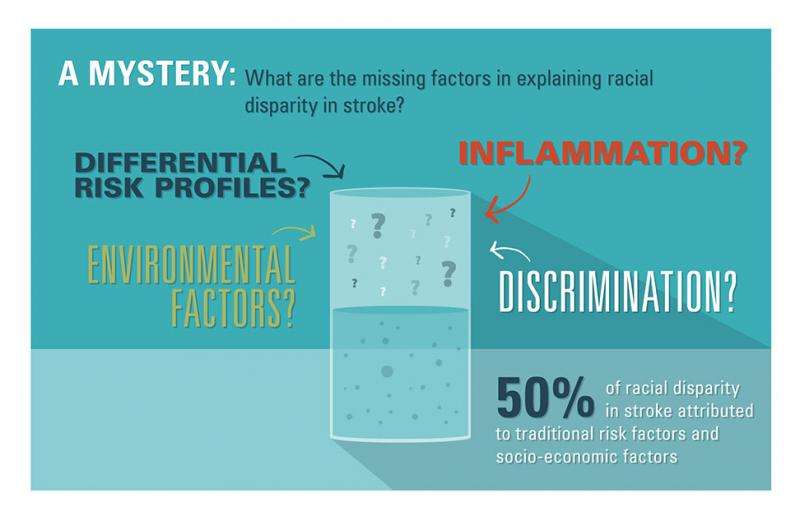
A mystery: What's missing?
For George Howard, the title of his 2011 paper in the journal Stroke sums up the major question to be answered in REGARDS' second decade: "Traditional Risk Factors as the Underlying Cause of Racial Disparities in Stroke: Lessons From the Half-Full (Empty?) Glass."
"We reported that approximately half of the racial disparity in stroke risk can be attributed to traditional risk factors and socioeconomic factors," he said. That gives physicians and policymakers a clear idea of how to make a major impact on reducing stroke disparities. But it also leaves a perplexing void.
"What other factors are contributing to this disparity?" George Howard said. "It could be that the same risk factors are worse for blacks than for whites, or it could be nontraditional risk factors, things like discrimination, environmental factors or inflammation."
"I think the biggest contribution of REGARDS is identifying that there is a lot we still don't know," said Virginia Howard. "We already know a lot about the importance of diabetes and hypertension. But we've shown that there's more out there."
The good news is that it isn't necessary to have the whole answer to do a great deal of good, George Howard adds. "If we can reduce the disparity between blacks and whites by just 5 percent, you're talking about huge numbers of people not having a horrible thing happen to them."

















