Saturated fat 'short-circuits' immune cells to trigger inflammation
Research by UC San Francisco scientists has opened up a surprising new avenue for potential therapies to reduce the risk of type 2 diabetes and other metabolic disorders that are associated with chronic tissue inflammation in obesity.
The researchers report that inflammation in obesity may be caused, at least in part, by a completely different mechanism from the one that controls normal immune responses. The research—published March 10, in the journal Cell Reports—shows that saturated fats "short-circuit" both mouse and human immune cells, producing an inappropriate inflammatory response as a consequence. This new pathway to inflammation can be blocked without interfering with the immune cells' normal response to infection-like signals, suggesting that it could be possible to develop drugs that reduce inflammation and diabetes risk in obesity without suppressing the immune system.
"This presents us with a fundamentally new way to think about how to prevent metabolic disorders linked to excess dietary fat from developing," said Suneil Koliwad, MD, PhD, an assistant professor in the Diabetes Center in UCSF's School of Medicine and senior author on the new paper.
For years, researchers have known that diet-induced obesity is often accompanied by inflammation in metabolic tissues such as fat, liver and muscle. Over time, this inflammation damages the tissues and may predispose some people to developing diabetes. There are currently few anti-inflammatory drugs under development to reduce this risk in obese patients, because such drugs also impair patients' immune systems overall, interfering with their ability to mount an inflammatory response following an injury or infection.
"These drugs are useful to alleviate symptoms of diseases like arthritis and may be able to slow down the course of diabetes," Koliwad said. "But the problem is that every time you get a cold you would have to come off the drug immediately."
The Role of Saturated Fats
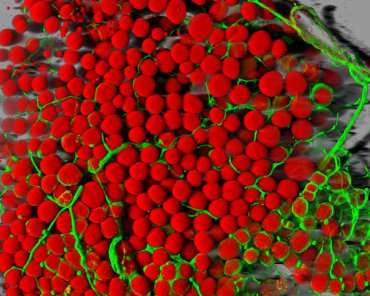
Koliwad's lab was initially investigating how genes and biochemical pathways in macrophages—a key inflammatory cell type in the immune system—are regulated by exposure to saturated fats of the type that are enriched in unhealthy diets.
Macrophages are usually thought of as the immune system's first-responders against disease, but they also are important in tissue repair and remodeling. In the case of obesity, when fat-storing cells become overloaded with fat and begin to fail, it's the macrophages' job to come in and dispose of the mess.
The researchers discovered that in mice, diets high in saturated fats activate a specific class of genes in macrophages that are separate from those responsible for detecting infection. In particular, they found that one gene, which encodes the protein IRE1alpha, is highly attuned to detect saturated fats that enter macrophages.
Studying macrophages in the lab, the team then found that IRE1alpha senses the accumulation of saturated fats and responds by communicating with a protein complex within the cell called the inflammasome. This protein complex triggers the production of an important inflammatory signal called IL-1beta, a long-time target of diabetes research.
Koliwad's group found that all the extra saturated fats that macrophages must suddenly process in obesity-like conditions essentially short-circuit IRE1alpha, whose normal role is to perform quality control and remodeling in a cells' protein production line, the endoplasmic reticulum. Blocking this fat-sensing function of IRE1alpha, the researchers discovered, prevented macrophages from turning on this inflammatory pathway in response to dietary fat, but had no impact on macrophages' ability to produce IL-1beta in response to signals associated with infection.
A Potential to Lower Inflammation Levels
To learn whether the same pathway is associated with obesity-triggered inflammation in humans, the researchers performed a meta-analysis of the literature and found a study in which immune cells from human blood were exposed to saturated fat and exhibited the same signature pattern of IRE1alpha activation.
The results from the Koliwad lab thus suggest a potential new approach to reducing IL-1beta and inflammation levels in patients with diet-induced obesity without the risks associated with global immunosuppression.
"There are thousands of studies each year on the effects of dietary compounds on cultured cells, and the challenge is always determining if those effects – seen in a very artificial setting – have any bearing on human health and disease," said Megan Robblee, a UCSF Biomedical Science graduate student and lead author on the new paper. "Although our study also has its caveats, we have the backing of the literature for the idea that saturated fats cause inflammation and that inflammation contributes to metabolic disease." The discovery of a mechanism that explains how these fats trigger inflammation through macrophages' IRE1alpha pathway simply fit in like a missing puzzle piece.
More information: Megan M. Robblee et al. Saturated Fatty Acids Engage an IRE1α-Dependent Pathway to Activate the NLRP3 Inflammasome in Myeloid Cells, Cell Reports (2016). DOI: 10.1016/j.celrep.2016.02.053


















