Why migration patterns are so important to designing responses to HIV
Significant strides have been made in the global response to HIV. But there is an urgent need to rethink the ways that prevention and treatment programmes are developed and implemented.
There is a body of knowledge that highlights the important role of migration and mobility in mediating the HIV epidemic in sub-Saharan Africa. Despite this, current responses fail to adequately engage the movement of people.
The policy and programme responses to HIV that are developed must be relevant for the different contexts of the continent. Population movement in the region is mostly associated with the search for improved livelihood opportunities. It involves a lot of internal movement of people who move within their country of birth.
South Africa receives the largest number of migrants from the region. Between 3% and 4% of the population is estimated to be cross-border migrants.
The relationship between people's mobility and local HIV epidemics must be taken into account.
But mobility should not merely be considered a risk factor. It should also be looked at as a structural determinant in how HIV responses are designed and implemented. This is because it has implications for the roll-out of pre-exposure prophylaxis and facilitates adherence to antiretroviral therapy.
Traditional patterns have changed
Population mobility has, historically, been a key driver in the early spread of the HIV epidemic on the continent.
But recent evidence suggests that national migration levels are no longer linked to national HIV prevalence or incidence in epidemics.
HIV risk profiles are instead associated with the individual movements of key populations.
Some migrants, for instance, reside in spaces of vulnerability such as transport corridors, urban informal settlements or mining hostels. These are areas associated with an increased risk of acquiring HIV.
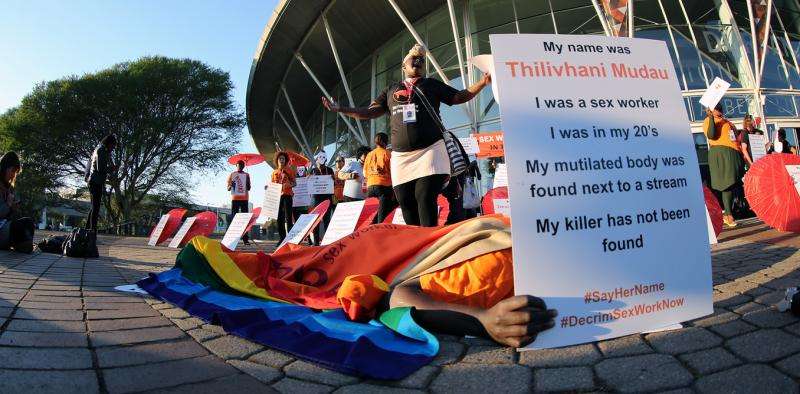
Certain mobile groups, including long-distance truck drivers and migrant sex workers are considered key populations at higher risk of acquiring HIV than the general population.
In a forthcoming chapter of the "Handbook of Migration and Health", Associate Professor Jo Vearey of the African Centre for Migration and Society argues that an improved and nuanced understanding of population mobility would help the fight against HIV. According to Vearey:
strengthening the understanding of the role of migration will assist in the development of migration-aware responses that are needed to support a more successful response to HIV in sub-Saharan Africa.
Vearey argues that there is a need to ensure that people living with HIV can access continued treatment regardless of their mobility trajectory.
The responses on the continent are limited
Regional and national responses often fail to engage with migration even in contexts where mobility is prevalent.
In South Africa, for example, the responses to the National Health Insurance green paper highlight the lack of consideration of migration and mobility to health responses at a national level.
Another example in the country is the National Strategic Plan for HIV.
Regionally, at the Southern African Development Community level, responses are limited. The 2009 Framework for Population Mobility and Communicable Diseases remains in draft form. The framework aims to harmonise responses to migration and HIV/TB/malaria within the region. The draft sits, despite the framework's proposed financing mechanism being finalised.
In most countries, and in the southern African region particularly, undocumented migrants face complex obstacles in accessing health-care services. These include HIV testing and antiretroviral therapy.
On the continent this is further compounded by the absence of regional job-seeker permits. The lack of effective systems to ensure treatment continuity such as the use of standardised patient-held records or cross-border referrals also play a role
A migration-aware response
The 2016 International AIDS Conference, themed "Access Equity Rights Now", urgently calls for extending HIV prevention, treatment and care services to those who still lack access. It also calls for HIV research and evidence-based interventions to be strengthened.
This should be coupled with the roll-out of pre-exposure prophylaxis to high-risk key populations such as sex workers – many of whom are migrants.
It certainly appears to be the best time for South Africa – and the sub-Saharan African region as a whole – to re-focus on poorly understood structural realities of HIV such as population mobility, and invest in migration-aware policy and programming.
Vearey argues that these programmes should support public health systems in the region to facilitate and respond to the movement of people. This movement can be within countries and across borders but should include anyone receiving antiretroviral therapy.
She also recommends that migration-aware HIV responses improve measures of migration and HIV prevalence. This would avoid unfounded automatic links between national and individual levels.
Programmes should look at disease-induced migration – where people move to seek treatment – such as HIV treatment-induced mobility.
"The Handbook of Migration and Health" will be published in December 2016 and made available via Edward Elgar Publishing.
This story is published courtesy of The Conversation (under Creative Commons-Attribution/No derivatives).
![]()
















