New-found stem cell helps regenerate lung tissue after acute injury, study finds
Researchers have identified a lung stem cell that repairs the organ's gas exchange compartment, according to a new study from the Perelman School of Medicine at the University of Pennsylvania. The y isolated and characterized these progenitor cells from mouse and human lungs and demonstrated they are essential to repairing lung tissue damaged by severe influenza and other respiratory ailments.
The research, led by Edward E. Morrisey, PhD, a professor of Cell and Developmental Biology, was published this week in Nature. Morrisey is also director of the Penn Center for Pulmonary Biology and scientific director of the Institute for Regenerative Medicine.
The development of the lung, or pulmonary system, is an evolutionary adaption to life on land. Lungs are essential in most large animals for a terrestrial existence. Their complex structure, which is dictated in part by their integration with the cardiovascular system, makes them an interesting yet difficult organ to study from a regeneration medicine perspective. In addition, lung disease is one of the leading causes of death in the world, surpassed only by cardiovascular disease and cancer.
"One of the most important places to better understand lung regeneration is in the alveoli, the tiny niches within the lung where oxygen is taken up by the blood and carbon dioxide is exhaled," Morrisey said. "To better understand these delicate structures, we have been mapping the different types of cells within the alveoli. Understanding cell-cell interactions should help us discover new players and molecular pathways to target for future therapies."
The Nature study examined the epithelial cells that line the surfaces of lung gas-exchange alveoli for stem cell behavior that could restore normal respiratory function after severe injury caused by an influenza infection or in such diseases as chronic obstructive pulmonary disease (COPD). While some organs, such as the intestine, turn over the entire epithelial lining every five days through the activity of a resident stem-cell lineage, organs such as the lung exhibit very slow turnover and contain stem cells that are activated only upon injury to regenerate the damaged tissue.
The team identified an alveolar epithelial progenitor (AEP) lineage which is embedded in a larger population of cells called alveolar type 2 cells, or AT2s. These cells generate pulmonary surfactant (a wetting agent), which keeps the lungs from collapsing upon every breath taken. "AEPs are a stable lineage in the lung and turn over very slowly, but expand rapidly after injury to regenerate the lining of the alveoli and restore gas exchange," said co-first author Will Zacharias, MD, PhD, a postdoctoral fellow in Morrisey's lab. David B. Frank, MD, PhD, a pediatric cardiologist at Children's Hospital of Philadelphia, is the other co-first author.
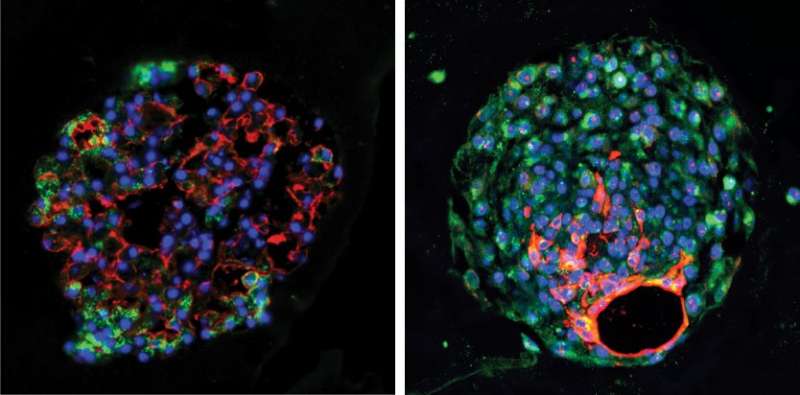
AEPs exhibit their own distinct suite of genes and contain a unique epigenetic signature. The Morrisey lab used the genomic information gained from mouse AEPs to identify a conserved cell surface protein called TM4SF1 that can be used to isolated AEPs from the human lung. Using this ability to isolate mouse and human AEPs, the team then generated David B. Frank three-dimensional lung organoids. "From our organoid culture system, we were able to show that AEPs are an evolutionarily conserved alveolar progenitor that represents a new target for human lung regeneration strategies," Morrisey said.
The team has access to more than 300 lungs through the lung transplant program headed by Edward Cantu, MD, an associate professor of Surgery. For their next study, the team aims to investigate influenza-damaged lung tissue as well as other lung disease models to determine where and when AEPs increase in response to acute lung injury or more chronic disease states.
Given the severity of the current influenza season, these studies provide new insight into how the human lung regenerates and identifies novel genetic and epigenetic pathways important for lung regeneration. The team is now exploring which of these molecular pathways may promote AEP function in the mouse and human lung, including understanding whether drugs designed to activate Fgf signaling, one of the key pathways conserved in mouse and human AEPs, may promote lung regeneration.
"We are very excited at this novel finding," said James P. Kiley, PhD, director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, which supported the study. "Basic studies are fundamental stepping stones to advance our understanding of lung regeneration. Furthermore, the NHLBI support of investigators from basic to translational science helps promote collaborations that bring the field closer to regenerative strategies for both acute and chronic lung diseases."
More information: Regeneration of the lung alveolus by an evolutionarily conserved epithelial progenitor, Nature (2018). DOI: 10.1038/nature25786













.jpg)






