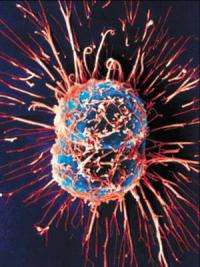
Dividing Cancer Cells. Credit: University of Birmingham
(PhysOrg.com) -- Every year, millions of people are diagnosed with cancer - a remarkably high number. But what about the flipside of those statistics? That is, two out of three people never get cancer, and more than half of heavy smokers don’t get cancer, either. A recent study points out this overlooked fact, and suggests that researchers might discover something by asking why so many people are resistant to the often deadly disease.
George Klein, Professor Emeritus at the Microbiology and Tumor Biology Center at the Karolinska Institute in Stockholm, Sweden, has been teaching and researching since the mid-1940s. In a recent study called “Toward a genetics of cancer resistance” published in the Proceedings of the National Academy of Sciences, Klein highlights evidence of several biological cancer resistance mechanisms that some individuals have that seem to prevent them from developing cancer. Perhaps, Klein says, there are cancer-resistant genotypes that “nip cancer in the bud” and keep most of us healthy.
As Klein explains, the suffering of cancer patients and their families has inspired most cancer researchers to focus on the genetics of cancer susceptibility. On the other hand, the genetics of cancer resistance has been largely unexplored, possibly because it is assumed to be merely the other side of the susceptibility coin. For example, if cancer is caused by mutations in genes that control cell division, then it logically seems that cancer resistance is simply a low occurrence of these mutations.
But, Klein says, maybe there is another alternative to the concept of cancer resistance. Perhaps most people have various protective mechanisms that counteract the development of cancer cells and stop the disease from progressing beyond the earliest stages.
“Cancer resistance must be investigated on its own merits,” Klein told PhysOrg.com. “It is possible and even likely that evolution has provided our species with highly efficient cancer resistance mechanisms. These may be the mechanisms that prevent most circulating, disseminated cancer cells that are found in the blood of all cancer patients to grow into metastasis, and can also nip cancerous foci (islands of cells in, for example, the prostate or the breast) in the bud, so that they do not progress.”
In a previous discussion, Klein and his coauthors identified five kinds of anticancer mechanisms. The first type is immunological, which applies to virus-associated cancers. For instance, researchers have compared the antibody responses of the squirrel monkey and the marmoset when infected with Herpesvirus saimri, a virus that is endogenous to squirrel monkeys but that the marmoset never encounters. When exposed to the virus, the marmosets, but not the squirrel monkeys, develop rapidly growing lymphomas. The researchers found a striking difference in the timing of each animal’s antibody response. In the tumor-resistant squirrel monkeys, the antibodies rose to a high level just three days after the infection, but, for the marmosets, the response took three weeks. By that time, the marmosets already had a rapidly growing virus-driven lymphoma. Research has shown that such immunological responses are influenced by genetic variation.
The second mechanism is genetic, and the most common example is DNA repair mechanisms. Studies have shown that there are individual variations in the efficiency of DNA repair, which is highlighted in cases such as the specific DNA repair deficiency called xeroderma pigmentosum. Individuals with this deficiency are highly sensitive to ultraviolet light, and even with careful protection they develop multiple skin carcinomas due to the genetic deficiency.
The third mechanism is epigenetic, which involve changes in gene expression, rather than changes in the DNA text itself. Studies have shown that when mice that carry a paternal precancerous mutation inherit a maternal imprinting defect, normal parental imprinting is impaired, which can increase the probability of cancerous development. In humans, this same imprinting defect occurs spontaneously and increases tumor incidence, affecting 10% of humans, and increasing their risk of intestinal cancer about threefold.
The last two anticancer mechanisms are intracellular and intercellular. As part of an intracellular defense, a cell can trigger apoptosis, or cell death, if it detects extensive DNA damage, so that the cell doesn’t reproduce and spread the damage. But sometimes, apoptosis isn’t triggered when it should be. For example, individuals who carry the genetically mutated tumor suppressor p53 run an increased risk of inheriting Li-Fraumeni syndrome, a rare disease in which patients develop multiple tumors.
Klein predicts that intercellular surveillance by neighboring cells, the fifth known anticancer mechanism, plays a major role in tumor resistance. Cells that are in direct physical contact with each other can detect precancerous conditions in one another, and together act as a microenvironmental control system to prevent the development and progression of unhealthy cells.
While the first four anticancer mechanisms are known to be influenced by genetic variation, little research has been performed on possible genetic or developmental variations in the efficiency of the intercellular anticancer mechanism. However, Klein mentions a group of largely forgotten experiments from the 1950s and ‘60s, where scientists crossed mouse strains that had a high incidence of cancer in a given tissue (due to inbreeding and selection for that particular type of cancer) with mice from a low incidence strain. In the experiments where they studied mammary cancer, hybrid females were taken from this case. Their own mammary glands were removed surgically. One mammary gland from the high cancer strain parent and one gland from the low cancer strain parent were then transplanted to two opposite flanks of the hybrids. Dealing with two inbred strains and their hybrid progeny, there is no problem with graft rejection, Klein explains.
It turned out that tumor incidence in the normal mammary gland derived from the high cancer parent was tenfold higher than in the mammary gland from the low cancer strain. Since both tissues were in the same host, exposed to the same hormonal and viral influences, it meant that the cancerous propensity of the high cancer strain and/or the resistance of the low cancer strain was at least partly inherited at the level of the tissue itself. This genetic difference could either act at the level of the cancer cells or at the level of their microenvironment.
Klein urges researchers to investigate this intercellular issue, along with the genetics of tumor resistance that act in multiple ways. Evolution seems to have favored some relatively common resistance genes that protect the majority of humans against cancer development. One day, finding out how nature keeps most of us cancer-free could help identify and repair specific genetic mechanisms in the large minority of individuals who do suffer from cancer. However, Klein says that it’s premature to speculate exactly how understanding genetic resistance could help people who are susceptible to cancer.
“First, it has to be shown that such protection mechanisms exist and, if so, what cellular and molecular mechanisms are responsible for them,” he said. “Only after that is clear, is it reasonable to ask whether this knowledge can be applied for the practical purpose of, for example, cancer prevention.”
More information: Klein, George. “Toward a genetics of cancer resistance.” PNAS, January 20, 2009, vol. 106, no. 3, 859-863.
Copyright 2008 PhysOrg.com.
All rights reserved. This material may not be published, broadcast, rewritten or redistributed in whole or part without the express written permission of PhysOrg.com.