Treatment for S. aureus skin infection works in mouse model
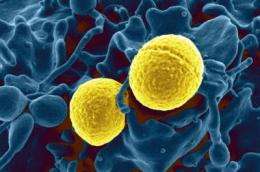
Scientists from the National Institutes of Health and University of Chicago have found a promising treatment method that in laboratory mice reduces the severity of skin and soft-tissue damage caused by USA300, the leading cause of community-associated Staphylococcus aureus infections in the United States.
By neutralizing a key toxin associated with the bacteria, they found they could greatly reduce the damaging effects of the infection on skin and soft tissue. Community strains of S. aureus cause infection in otherwise healthy people and are considered extremely virulent, as opposed to hospital strains that infect people who already are weakened by illness or surgery.
While much recent attention has been focused on deaths caused by S. aureus infection in the bloodstream—and those caused by methicillin-resistant S. aureus in particular—the Centers for Disease Control and Prevention estimates that in 2005, physicians treated 14 million non-lethal S. aureus skin and soft-tissue cases in the United States.
In their study, now online in The Journal of Infectious Diseases, scientists from NIH's National Institute of Allergy and Infectious Diseases (NIAID) examined the effects of the bacterial toxin alpha-hemolysin, or Hla, on S. aureus skin infections in laboratory mice. In all aspects of the study where the Hla toxin was either removed from S. aureus bacteria or neutralized through immunization, skin abscesses were significantly smaller, mice recovered faster and there was little or no skin destruction.
When S. aureus secretes Hla during infection in humans, the toxin pokes holes in a variety of different host cells, killing them. Scientists who have studied Hla for years have mainly focused on neutralizing the toxin in cases of pneumonia-related S. aureus infection. Until now, no one had tested how the absence of Hla would affect the severity of USA300 skin infections and whether immunization against the toxin could neutralize Hla and its contribution to the severity of skin disease.
"For cases of skin and soft-tissue infection caused by Staph aureus, this study highlights the potential for antitoxin treatment to become an effective alternative to traditional antibiotics, which we know have limitations because of drug resistance," says NIAID Director Anthony S. Fauci, M.D. Antitoxins prevent harm caused by a specific part of a pathogen—such as Hla in S. aureus—rather than trying to kill the entire pathogen, as antibiotics do.
The study, led by Frank DeLeo, Ph.D., of NIAID's Rocky Mountain Laboratories in Hamilton, Mont., documented physical differences in mice infected with different strains of S. aureus, including USA300 with or without Hla. The second portion of the study tested what is known as active and passive immunity, with mice being immunized with a non-lethal version of the toxin or injected with Hla-specific antibodies, respectively. Both types of immunization protected mice from skin lesions that typically destroy skin and surrounding tissue.
The group noted that multiple S. aureus molecules must contribute to skin infection because simply removing or neutralizing Hla did not completely prevent the formation of skin abscesses, although the abscesses were smaller in size.
Study collaborators from the University of Chicago, Olaf Schneewind, M.D., Ph.D., and Juliane Bubeck Wardenburg, M.D., Ph.D.,contributed the Hla treatment concept, which they developed through their recent work on S. aureus pneumonia. Dr. DeLeo's group adapted that work to their mouse model of skin infection, which is a good indicator of how abscess size and skin destruction could affect humans, according to the study investigators.
"This toxin is probably one of the most promising targets we currently have in our efforts to develop therapeutics that protect against severe Staph aureus skin infections," says Dr. DeLeo. His group is continuing its collaboration with Drs. Schneewind and Bubeck Wardenburg on the project.













