New radioisotope will improve cancer therapy
The high neutron flux at the Institut Laue-Langevin (ILL) has produced samples of 161Tb, an isotope of terbium with better properties for cancer therapy than existing radiopharmaceutical treatments. Researchers led by Paul Scherrer Institute (PSI) and collaborating with ILL and Technical University of Munich, confirmed that 161Tb could be produced in sufficient quantity and quality for therapeutic use.
Radiopharmaceuticals (where a radioactive isotope is attached to a bioconjugate that selectively delivers it to cancer cells) are one of the best ways to diagnose and treat tumours. Radiopharmaceuticals are already very successful in fighting certain types of cancer, but those isotopes currently in use are not optimal for all therapeutic applications. They may cause collateral damage to healthy tissue or require an isolation of the patient during treatment. Better isotopes exist but are not commercially available. Advance in this field is crucially dependant on the availability of innovative isotopes for initial R&D, and then on the capability to produce large quantities for clinical applications. Today’s 161Tb research is therefore an important step towards a new treatment that might improve the quality of cancer treatment and patient care.
What’s so great about 161Tb?
“We have developed an innovative radiochemical method for the production of the novel therapeutic radioisotope 161Tb with highest quality suitable for medical applications. The production is scalable to provide enough 161Tb for the treatment of hundreds of patients per week.” says Dr Konstantin Zhernosekov, Head of the Radionuclide Development Research Group at PSI.
161Tb has desirable decay properties for use in cancer therapy:
• Half life of 6.9 days – long enough to transport to hospitals but short enough not to pose long term issues of waste handling after excretion from the patient
• Emits low-energy β particles and low-energy electrons – results in a short cytotoxic range with minimal collateral damage to healthy tissue
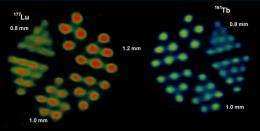
• Emits a small amount of gamma radiation – enough to detect exactly where the radioisotope has been delivered to 161Tb has the same preparation protocol to attach it to the bioconjugate, and very similar biochemistry and metabolism, as 177Lu (an isotope of lutetium), one of the newest, commercially available radioisotopes for treatment. It also has similar β emissions to 177Lu, but emits more low-energy (Auger) electrons, which mean it would be more effective for treating tumours of a small size. 177Lu is already in use in several European countries, a well as Australia, Brazil and others, which should smooth the way for 161Tb.
“The development of new, better targeted, bioconjugates should be coupled with radioisotopes that have more targeted (ie short-range) radiation. The ultimate treatment would be Auger electron emitters, that would just destroy the cancer cell without harming neighbouring cells,” says Dr Ulli Köster, physicist at ILL. ”Doctors and regulators are understandably cautious when it comes to new therapies. 161Tb has the advantage of combining β radiation (whose effects are well-known) with additional Auger electron emission. The fact that 161Tb also has very similar in vivo behaviour to 177Lu, and is prepared and handled in the same manner, will be reassuring for the medical professionals, and so should pave the way for Auger electron therapy.”
"Neuroendocrine tumors develop from hormone producing cells and occur in particular in the gastrointestinal tract and the lung. They have a wide spectrum, may develop slowly or rapidly and create metastases. Using nuclear medical treatment we have obtained a dramatic improvement in how the disease progresses in patients. We strongly embrace increasing the choice of available radioisotopes. We would like to use 161Tb, the first samples of which were produced at ILL, in clinical therapy. We are very delighted about this progress in basic research that will yield a direct outcome for cancer therapy". says Prof Richard Baum, Head of the Clinics for Nuclear Medicine / PET-Center, Zentralklinik Bad Berka GmbH.
The future
ILL is developing technical plans for an automated irradiation system to routinely produce 161Tb, 177Lu and other innovative radioisotopes for medical use. If financial backing is found and regulatory approval is obtained the system would become operational in 2013.
Prof Andrew Harrison, Science Director of ILL: “ILL’s intense neutron flux – among the three most intense research reactors worldwide – means we are one of few places in the world with the capability to produce high quality isotopes for radiotherapy research and development. The proposed irradiation system is outside of ILL’s normal sphere of activity, but we have a moral imperative to do this work. It’s a great example of how a publicly funded facility can have a totally unexpected and unpredictable payoff for society.”
Prof Mikael Jensen, researcher and QP at The Hevesy Laboratory, Risø-DTU, Technical University of Denmark, said: “Nuclear medicine is extremely successful for diagnosis – we get better and better at imaging, but treatment hasn’t progressed as quickly. We were looking for the magic bullet among biovectors, but it’s difficult to find one that is selective for cancer cells and highly cytotoxic. Therefore, we’re now combining them with something that is only dangerous to cells if gets inside them – certain radioisotopes. 161Tb is a good tool for this as it has the right decay properties, and we already know the chemistry. By proving that 161Tb can be made in sufficient quantity and quality, this research provides another small handle on how to deal with the complex and many-headed beast that is cancer. Medical doctors are already familiar with soft β emitters, so even if they don’t know 161Tb by name they’ll appreciate it’s potential.”















