New model of childhood brain cancer establishes first step to personalized treatment
Scientists at Sanford-Burnham Medical Research Institute (Sanford-Burnham) developed a new mouse model for studying a devastating childhood brain cancer called medulloblastoma. The animal model mimics the deadliest of four subtypes of human medulloblastoma, a tumor that is triggered by elevated levels of a gene known as Myc. The study, published February 13 in the journal Cancer Cell, also suggests a potential strategy for inhibiting the growth of this tumor type. This achievement marks an important milestone toward personalized therapies tailored to a specific type of medulloblastoma.
"Being able to use an animal model as a tool to test treatments has been very valuable in medulloblastoma, as in other types of tumors. But for Myc-associated tumors, that hasn't been an option because there hasn't been a model of the disease. This is the first step to developing therapies for this type of tumor," said Robert Wechsler-Reya, Ph.D., director of the Tumor Development Program in Sanford-Burnham's National Cancer Institute-designated Cancer Center, member of the Sanford Consortium for Regenerative Medicine, and senior author of the study.
Children with medulloblastoma develop tumors in a region of the brain called the cerebellum, which plays an important role in motor control. Seventy-five percent of children with the disease survive after aggressive surgery, radiation, and chemotherapy—but, according to Wechsler-Reya, side effects can be severe, leading to cognitive deficits, endocrine disorders, and the development of other cancers later in life.
In this latest study, Wechsler-Reya, postdoctoral researcher Yanxin Pei, Ph.D., and colleagues showed that cerebellar stem cells engineered with the Myc oncogene initially gave rise to large masses of cells when transferred to mice, but after four weeks these cells disappeared. Researchers have known for years that the Myc oncogene causes cells to grow but also, paradoxically, to die. The reason is that Myc activates another gene called p53, which senses that something is wrong with the cell and causes it to self-destruct. The next step was to inactivate p53, which the researchers did by giving the cells a mutant form of the gene to block its effects.
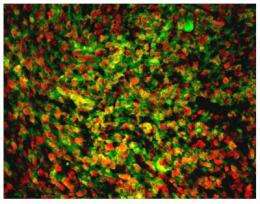
The result was striking: the newly engineered cerebellar stem cells, carrying Myc and mutant p53, formed large tumors in mice that continued to grow over time. Moreover, these tumors resembled those seen in humans with Myc-driven medulloblastoma.
The researchers then profiled the genes that are expressed in the tumors and found particularly high levels of genes that are activated by an enzyme called PI3-kinase. PI3-kinase is an important part of the mechanism that cells use to stay alive, and its activity is often elevated in cancer cells. Armed with this information, the team tested whether inhibiting PI3-kinase could block the growth of Myc-driven tumors.
"We found that PI3-kinase inhibitors significantly increased mouse survival," said Pei, the study's first author.
PI3-kinase inhibitors are in clinical trials for several types of cancer, but no one has tried them as a treatment for medulloblastoma. Wechsler-Reya said his lab is now taking steps toward testing these inhibitors as a potential therapy for the disease.
"Obviously there are many steps between screening compounds in the lab and giving drugs to patients," Wechsler-Reya said. "But some of the steps can be cut short if you use drugs that are already in trials or in use for other diseases."
The team plans to screen other compounds using the new mouse model to test their effectiveness in stopping tumors. Wechsler-Reya's lab is also working on developing new mouse models to study other medulloblastoma subtypes.
"The key is to take compounds that show promise in pre-clinical studies in the lab and partner with clinicians to evaluate their effectiveness in the clinic," Wechsler-Reya said. "Our hope is that this approach will bring new therapies to children who are suffering from this extremely aggressive disease."














