Culprit behind unchecked angiogenesis identified
German researchers unravel a critical regulatory mechanism controlling blood vessel growth that might help solve drug resistance problems in the future.
Angiogenesis, the growth of new blood vessels, is a complex process during which different signalling proteins interact with each other in a highly coordinated fashion. The growth factor VEGF and the Notch signalling pathway both play important roles in this process. VEGF promotes vessel growth by binding to its receptor, VEGFR2, while the Notch signalling pathway acts like a switch capable of suppressing angiogenesis. Until recently, scientists had assumed that Notch cancels the effects of VEGF through the downregulation of VEGFR2. Now, researchers at the Max Planck Institute for Molecular Biomedicine and the Westphalian Wilhelms-University in Münster, Germany, were able to demonstrate that defective Notch signalling enables strong and deregulated vessel growth even when VEGF or VEGFR2 are inhibited. In this case, a different VEGF family receptor, VEGFR3, is strongly upregulated, promoting angiogenesis. "This finding might help explain drug resistance issues in certain types of cancer therapy and could become the basis for novel treatment strategies," suggests Ralf Adams, MPI's Executive Director and Chair of the Department of Tissue Biology and Morphogenesis.
An extensively branched network of blood vessels provides every organ of the body with nutrients and removes harmful metabolic waste products from tissues. Growth of this vascular system is essential for development and wound healing processes. Uncontrolled angiogenesis contributes to diseases like hemangiomas, the sponge-like overgrowth of blood vessels in the skin, or retinopathies impairing the eyesight of diabetic and elderly individuals. In cancer therapy, inhibition of angiogenesis is used to starve tumours and prevent the metastatic spread of cancer cells via the circulation. At present, this is most frequently done by targeting VEGF or its receptor VEGFR2. When their oxygen supply becomes inadequate, tissues begin to release VEGF, which binds to VEGFR2, activating the receptor and thereby triggering vessel growth. Thus, the formation of new blood vessels can be blocked by inhibiting VEGF or VEGFR2. Unfortunately, existing treatments are inadequate and, for reasons that are not yet known, some patients respond poorly or not at all to VEGF/VEGFR2 inhibition.
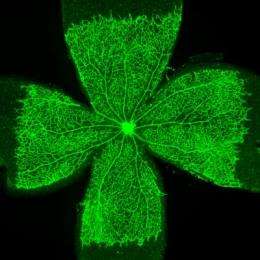
Now, Rui Benedito, a postdoctoral research fellow in Adams' Department, has demonstrated that inhibition of the Notch pathway in blood vessels of the mouse eye permits strong and deregulated vessel growth even when VEGF or VEGFR2 are inhibited. "It turns out that another VEGF family receptor, VEGFR3, takes over, promoting the formation of new blood vessels," explains Benedito. VEGFR3 is strongly upregulated in blood vessels in the absence of Notch and is active even without growth signals from the surrounding tissues.
"What we need to do now is confirm whether VEGFR3 and other Notch-regulated signals are in fact capable of promoting VEGF-independent vessel growth in eye disease or cancer not only in mice but also in humans," explains Adams. "It might become possible to predict whether patients, depending on their vascular Notch activation status, are going to respond to VEGF or VEGFR2 inhibition. This would allow physicians to choose alternative therapies if necessary. Here, too, collaboration between MPI, the medical faculty, and the University of Münster is essential: "Our work is strongly benefitting from the excellent support provided by the University."
More information: Rui Benedito, Susana F. Rocha, Marina Woeste, Martin Zamykal, Freddy Radtke, Oriol Casanovas, Antonio Duarte, Bronislaw Pytowski & Ralf H. Adams Notch-dependent VEGFR3 upregulation allows angiogenesis without VEGF–VEGFR2 signalling. Nature, DOI: 10.1038/nature10908
















