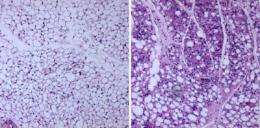
Sections of white fat taken from normal mice (left) and from mice without an enzyme called fatty acid synthase (FAS) in their fat cells (right). Mice without FAS can eat a high-fat diet without becoming obese. Credit: Semenkovich lab
Researchers at Washington University School of Medicine in St. Louis have identified a potential target for treating diabetes and obesity.
Studying mice, they found that when the target protein was disabled, the animals became more sensitive to insulin and were less likely to get fat even when they ate a high-fat diet that caused their littermates to become obese.
The findings are published online in the journal Cell Metabolism.
The researchers studied how the body manufactures fat from dietary sources such as carbohydrates. That process requires an enzyme called fatty acid synthase (FAS). Mice engineered so that they don't make FAS in their fat cells can eat a high-fat diet without becoming obese.
"Mice without FAS were significantly more resistant to obesity than their wild-type littermates," says first author Irfan J. Lodhi, PhD. "And it wasn't because they ate less. The mice ate just as much fatty food, but they metabolized more of the fat and released it as heat."
To understand why that happened, Lodhi, a research instructor in medicine, analyzed their fat cells. Mice have two types of fat: white fat and brown fat. White fat stores excess calories and contributes to obesity. Brown fat helps burn calories and protects against obesity.
Researchers at Washington University School of Medicine in St. Louis have identified a potential target for treating diabetes and obesity. They discovered that when a particular protein is disabled in mice, they get more sensitive to insulin and less likely to become fat, even when they eat a high-fat diet. Credit: Washington University BioMed Radio
In mice genetically blocked from making fatty acid synthase in fat cells, Lodhi and his colleagues noticed that the animals' white fat was transformed into tissue that resembled brown fat.
"These cells are 'brite' cells, brown fat found where white fat cells should be," Lodhi says. "They had the genetic signature of brown fat cells and acted like brown fat cells. Because the mice were resistant to obesity, it appears that fatty acid synthase may control a switch between white fat and brown fat. When we removed FAS from the equation, white fat transformed into brite cells that burned more energy."
Determining whether humans also have brown fat has been somewhat controversial throughout the years, but recent studies elsewhere have confirmed that people have it.
"It definitely exists, and perhaps the next strategy we'll use for treating people with diabetes and obesity will be to try to reverse their problems by activating these brown fat cells," says senior investigator Clay F. Semenkovich, MD.
Semenkovich, the Herbert S. Gasser Professor of Medicine, professor of cell biology and physiology and director of the Division of Endocrinology, Metabolism and Lipid Research, says the new work is exciting because FAS provides a target that may be able to activate brown fat cells to treat obesity and diabetes. But even better, he says it may be possible to target a protein downstream from FAS to lower the risk for potential side effects from the therapy.
That is possible because the scientists learned that the FAS pathway involves a family of proteins known as the PPARs (peroxisome proliferator-activated receptors). PPARs are important in lipid metabolism. One of them, PPAR-alpha, helps burn fat, but the related protein, PPAR-gamma manufactures fat and helps store it.
Lodhi and Semenkovich noticed that in mice without FAS in their fat cells, activity of PPAR-alpha (the fat burner) was increased, while PPAR-gamma (the fat builder) activity decreased.
A protein called PexRAP (Peroxisomal Reductase Activating PPAR-gamma) turned out to be a downstream mediator of the effects of FAS and a key regulator of the PPAR-gamma, fat-storing pathway. When the researchers blocked PexRAP in fat cells in mice, they also interfered with the manufacture and buildup of fat.
"There was decreased fat when we blocked PexRAP," Lodhi says. "Those mice also had improved glucose metabolism, so we think that inhibiting either fatty acid synthase or PexRAP might be good strategies for treating obesity and diabetes."
Several pharmaceutical companies are working on FAS inhibitors. Meanwhile, the discovery that inhibiting PexRAP also makes the animals less obese and less diabetic has convinced the Washington University researchers to continue those studies.
"Because PexRAP is downstream, it theoretically might cause fewer side effects, but nobody knows what role the protein might play in different tissues in the body," Semenkovich says. "We need to conduct more experiments with the goal that we may be able to move into some sort of clinical trials relatively soon. It's very important to find new treatments for obesity and diabetes because these disorders aren't just an inconvenience, both can be lethal."
More information: Lodhi IJ, Yin L, Jensen-Urstad APL, Funai K, Coleman T, Baird JH, El Ramahi MK, Razani B, Song H, Fu-Hsu F, Turk J, Semenkovich CF. Inhibiting adipose tissue lipogenesis reprograms thermogenesis and PPARγ activation to decrease diet-induced obesity. Cell Metabolism, vol. 16 (2), Aug. 8, 2012.
Journal information: Cell Metabolism
Provided by Washington University School of Medicine