April 30, 2013 report
Making a window for drug delivery in the blood-brain barrier
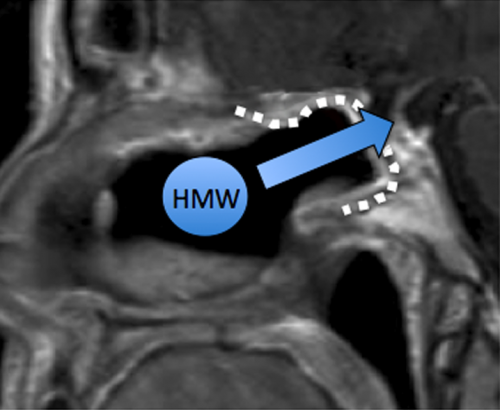
(Medical Xpress)—The blood-brain barrier (BBB) prevents most large or hydrophilic (polar) molecules from getting into the brain. For many neurological diseases, like Parkinson's, the presence of the BBB severely limits treatment options. Methods to get around the BBB, by using protein conjugated drugs, or even transcranial catheters, have been of limited practical use. Taking a cue from an established surgical technique used to access the brain to remove pituitary tumors, researchers in Boston have come up with a method to create a permanent window in the BBB, which can be used to administer drugs. Their paper, just published in PLOS ONE, describes how to graft semipermeable nasal mucosa into a surgical gap made in the bone at the back of the nose.
Normally, the circulatory system of the body is isolated by tight junctions between the endothelial cells of the capillaries inside the brain. There is also a thick basement membrane composed of matrix proteins, as well as astrocytic endfeet surrounding the capillaries. Nutrients required by the brain, such as glucose and amino acids, are actively transported across this barrier by specific membrane-bound transporter proteins. There are also specific efflux pumps, that remove certain molecules that might occasionally breach the BBB.
Endoscopically accessing the brain through the nose has made many difficult surgeries routine. Removing tumors from normally inaccessible regions, like the pituitary, can now be done with little risk. Typically these procedures require removal of intervening dura mater and arachnoid membrane, which creates a significant communication between the inside of the nose and the surface of the brain. To seal up the gap, nasal mucosal grafts are harvested from the nasal septum. When healed, these grafts can potentially provide a means to bypass the BBB and permit high molecular weight or polar molecules to get into the brain.
To determine the diffusion capacity of transplanted nasal mucosa, the researchers applied fluorescent rhodamine-dextran molecules of different sizes to a mouse graft model. Dextran polymer molecular weights of 20, 40 and 500 kDa were tested. All three weights showed significant penetration into the brain which peaked at around 72 hours. The grafts proved to be water tight, immunocompetent, and permanent, suggesting they may be a viable way to create a drug-permeable window for humans.
The trans-olfactory drug delivery route has been studied previously in rats, and it was found that nerve growth factor (NGF) could be absorbed in significant doses. Unfortunately, these finding failed to translate into a clinical success in humans. One reason for the the failure may be due to the relatively small size and distribution of the olfactory mucosa in humans. The researchers in the present study did look at the striatum, a region important for the treatment of Parkinson's disease. They found penetration of fluorescent dextran into this region, suggesting potential therapeutic benefit in humans may be possible.
Intranasal drug delivery to the CNS is currently utilized in Parkinson's treatment to deliver apomorphine, although its ultimate utility has been controversial. The mucosal graft procedure described here would have to be further vetted before it would ready for actual clinical trials. One concern would be the possibility for sinus or other infection to propagate through the graft, particular over longer periods of time. Convection and natural CSF circulation is also different in the brains of mice and humans, in addition to the disparity of scale. However when contrasted with the infection risk inherent in using catheters or cannulas to deliver drugs into the brain, the transplanted olfactory mucosa route has plenty of appeal.
More information: Bleier BS, Kohman RE, Feldman RE, Ramanlal S, Han X (2013) Permeabilization of the Blood-Brain Barrier via Mucosal Engrafting: Implications for Drug Delivery to the Brain. PLoS ONE 8(4): e61694. doi:10.1371/journal.pone.0061694
Abstract
Utilization of neuropharmaceuticals for central nervous system(CNS) disease is highly limited due to the blood-brain barrier(BBB) which restricts molecules larger than 500Da from reaching the CNS. The development of a reliable method to bypass the BBB would represent an enormous advance in neuropharmacology enabling the use of many potential disease modifying therapies. Previous attempts such as transcranial catheter implantation have proven to be temporary and associated with multiple complications. Here we describe a novel method of creating a semipermeable window in the BBB using purely autologous tissues to allow for high molecular weight(HMW) drug delivery to the CNS. This approach is inspired by recent advances in human endoscopic transnasal skull base surgical techniques and involves engrafting semipermeable nasal mucosa within a surgical defect in the BBB. The mucosal graft thereby creates a permanent transmucosal conduit for drugs to access the CNS. The main objective of this study was to develop a murine model of this technique and use it to evaluate transmucosal permeability for the purpose of direct drug delivery to the brain. Using this model we demonstrate that mucosal grafts allow for the transport of molecules up to 500 kDa directly to the brain in both a time and molecular weight dependent fashion. Markers up to 40 kDa were found within the striatum suggesting a potential role for this technique in the treatment of Parkinson's disease. This proof of principle study demonstrates that mucosal engrafting represents the first permanent and stable method of bypassing the BBB thereby providing a pathway for HMW therapeutics directly into the CNS.
© 2013 Medical Xpress
















