Oncogene mutation hijacks splicing process to promote growth and survival
An international team of researchers – led by principal investigator Paul S. Mischel, MD, a member of the Ludwig Institute for Cancer Research and professor in the Department of Pathology at the University of California, San Diego School of Medicine – has found that a singular gene mutation helps brain cancer cells to not just survive, but grow tumors rapidly by altering the splicing of genes that control cellular metabolism.
The findings are published online in the journal Cell Metabolism.
Mischel, who heads the Ludwig Institute's molecular pathology laboratory based at UC San Diego, and colleagues focused upon a process called alternative splicing, in which a single gene encodes for multiple proteins by including or excluding different, specific regions of DNA.
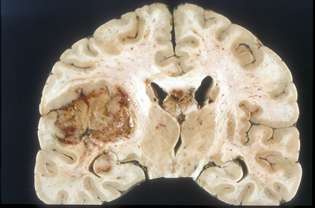
Alternative splicing is a tightly regulated and normal activity in healthy cells. For Mischel and colleagues in Los Angeles, Ohio and Japan, the question was whether mutations of a gene called EGFRvIII caused differential alternative splicing in glioblastoma multiformes (GBMs), the most common and aggressive type of malignant brain tumor. Median survival after GBM diagnosis is just 15 months with standard-of care radiation and chemotherapy. Without treatment, it is less than five months.
The scientists were particularly interested in whether the EGFRvIII mutation induced alternative splicing events that resulted in deregulation of normal cellular metabolism. "We focused on the 'Warburg Effect,' a common metabolic derangement in cancer that enables tumor cells to metabolize glucose in a way that provides both a sufficient supply of energy and a source of building blocks that can be used for growth," Mischel said.
They discovered a complex but compelling series of consequential events: The EGFRvIII mutation controls expression of a splicing factor called HNRNPA1, which initiates an alternatively spliced form of a regulatory protein called Max. The alternative form is called Delta Max.
Max is associated with MYC, a gene that drives tumor growth and the Warburg Effect in cancer. "Unlike the regular form of Max," said Mischel, "Delta Max actually enhances c-MYC activity, specifically by promoting the glycolytic phenotype of the tumor cells." In other words, the EGFRvIII mutation and subsequent alternative splicing commandeer the cell's metabolic machinery in a way that lets it take up and use glucose to promote rapid tumor growth.
Mischel noted that the findings are specific to the EGFRvIII mutation and GBMs. It's not known whether other oncogenes are able to exploit alternative splicing in similar fashion.
The findings, according to Mischel, provide two clear insights. First, they highlight the central role of EGFRvIII in GBM pathogenesis and its critical role in altering cellular metabolism in tumors. Second, they show that oncogenes can regulate cell metabolism through alternative splicing, which may provide a new set of targets for oncogene-specific drug development.















