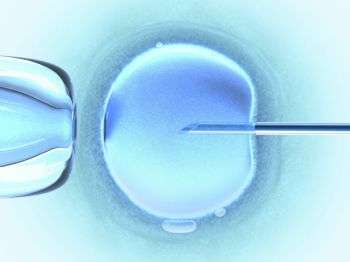
A human ovum is fertilised using IVF techniques
(Medical Xpress)—Three evolutionary biologists with ties to research facilities in the U.K., Germany and Australia have published a Policy Forum piece in the journal Science suggesting that governmental agencies slow the rush to allow mitochondrial replacement (MR) therapy to undergo clinical trials. A trial is currently on track in the U.K. that could lead to the in vitro fertilization (IVF) technique being made available to the British public as early as 2015.
MR has been developed as a means of helping people with mitochondrial mutations have healthy babies. Women with such mutations tend to have babies with a wide variety of ailments which quite often prevent them from surviving into adulthood. MR involves removing the pronuclei from a fertilized embryo and inserting it into an embryo that has been donated by another woman—the pronuclei from the donor embryo is discarded. The end result is a single embryo with the original mother's pronuclei and the donor's mitochondria—placed into the womb of the original mother leading to the birth of a child. Thus far the technique has led to the birth of four offspring by a macaque mother—who are now three years old. Testing in humans has only gone so far as the blastocyst stage, approximately 5 days after fertilization. Because results so far have shown such promise, the U.K.'s IVF governing body, Human Fertilisation and Embryology Authority, wants to start clinical trials of the technique using volunteer women, as soon as possible.
Klaus Reinhardt, Damian Dowling and Edward Morrow write in Science, that they are concerned that the rush to clinical testing might be premature. They suggest the government wait for more research to be conducted before running trials that could conceivably result in babies being born with birth defects. At issue is the DNA present in mitochondria—though there is just a very small amount of it, the researchers are worried that not enough testing has been conducted regarding its interaction with the DNA found in the pronuclei. They point out that some research has suggested there may be problems with matching in some circumstances leading to birth defects. They note also that the macaque offspring haven't even reached adulthood yet, which means no one yet knows if they will develop defects, such as problems with fertility.
The trio is not suggesting work be stopped on the technique or that it's dangerous, immoral or wrong (as others have claimed), they simply believe that more time should be devoted to testing before taking a leap of faith that the technique will work as hoped in humans, resulting in a human being who had no say in the decision making process.
More information: Mitochondrial Replacement, Evolution, and the Clinic, Science 20 September 2013: Vol. 341 no. 6152 pp. 1345-1346 DOI: 10.1126/science.1237146
Abstract
Mitochondrial diseases [often caused by mutations in mitochondrial DNA (mtDNA)] can manifest in a range of severe symptoms, for which there are currently no cures (1). The diseases are passed from mothers to offspring. Intense research efforts have recently focused on a germline therapeutic strategy to prevent the inheritance of disease-causing mitochondria. However, although there has been increased government interest, especially in the United Kingdom, for using this approach to treat patients, there are reasons to believe that it is premature to move this technology into the clinic at this stage.
Journal information: Science
© 2013 Medical Xpress