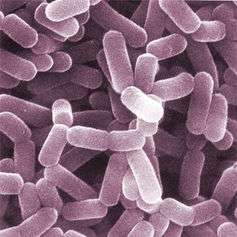
The trillions of bacteria in your gut can affect your brain – psychologically and physically. Credit: Helga Weber
Striking new evidence indicates that the gut microbiome, the ecological community of microorganisms that share our body, has a huge effect on brain function – much larger than we thought.
It has long been established that our gut acts as a second nervous system and is capable of functioning without input from the brain.
Nevertheless, the brain and gut are still intimately connected through a process called "the gut-brain axis", and changes to either system can have dramatic effects on the other.
The guts of both vertebrate and invertebrate animals are home to trillions of microorganisms, which primarily consist of mutualistic bacteria.
These resident bacteria play an essential role in many of our biological processes, such as supplying important nutrients, breaking down indigestible compounds and defending against other pathogenic microbes.
Bacterial composition has recently been correlated with several neurological disorders, especially those relating to anxiety. While the exact way gut microbes affect the nervous system is unfortunately not yet entirely understood, scientists are working to answer this question by exploring brain function at the molecular level.
How do gut microbes affect the brain?
Two research teams headed by Rochellys Diaz Heijtz and Thomas Neufeld recently discovered that completely eliminating gut bacteria from mice had surprising effects on the animals' anxiety levels.
When tested under conditions that would normally induce stress, bacteria-free mice were found to have significantly less anxiety and anxiety-associated behaviours than the mice with normal intestinal microbes. This was one of the first instances showing that the gut microbes may play a role in mental disorders.
To investigate why removing the gut microbiome correlated with reduced anxiety, both teams explored the possibility that gut bacteria may influence the activation of genes important for brain function.
Credit: Aaron Logan
Specifically, the activity of genes involved in regulating neuron survival and signalling—along with genes that encode for receptors that bind important neurotransmitters - were changed. For instance, several neurotransmitters, including serotonin, were altered within regions of the brain associated with motor control and anxiety-like behaviour in bacteria-free mice.
This hints that intestinal bacteria have some level of influence on DNA transcription – especially on genes that are essential for brain function.
Gut flora may also alter the way the brain changes during the earliest stages of life. Young, microbe-free mice were reconstituted with normal levels of intestinal flora to examine how these bacteria affects neurogenesis, the process where neurons are generated from stem cells and progenitor cells during pre-natal development.
As a result of these tests, activation of genes responsible for the maturation of neurons was found to be increased. This demonstrates that gut flora may be essential for proper brain development during the foetal stage.
Gut bacteria, therefore, seems to play an essential role in neuronal growth. As bacteria colonise the gut in the days following birth – a sensitive period for brain development – poor establishment of the microbiome may potentially lend to the occurrence of anxiety-based disorders.
The key players: identifying important bacteria
While these studies have revealed that removing our gut microbes has serious effects on the brain, it begs the questions of whether specific types of bacteria are more important for neural function than others. This is becoming clear as scientists explore brain changes associated with some of our most common species.
For instance, in 2011, researchers in Ireland discovered that mice treated with the common probiotic bacterium Lactobacillus rhamnosus had reduced stress hormone and anxiety related behaviours.
L. rhamnosus was later found to influence gamma-Aminobutyric acid (GABA), the primary central nervous system inhibitory neurotransmitter involved in regulating countless processes.
Lactobacillus bacteria. Credit: AJ Cann
GABA or GABA receptors are associated with the development of anxiety and depression, suggesting that this particular probiotic helps to normalise GABA in the brain and consequently reduce stress.
Microbes as a treatment option
Together, these recent findings highlight the important role of bacteria in the communication between the gut and the brain. Our increasing knowledge of how human mental illnesses – such as autism, anxiety, and depression – are linked to gut flora may lead to future treatments of mental illness.
This could include administration of probiotics or faecal transplant procedures that would modify gut flora community structures. Already, studies doing exactly this through clinical trials show promising results, with many patients reporting improved mental health after high-dose treatments.
Our knowledge of this specific area of neuroscience is expanding quickly, but in order to advance this emerging field of medical research, we will require experimental approaches that more accurately describe the microbial community of the gut and identify other behaviour-modifying species.
In addition, experiments that seek to either alter microbial communities or the molecular signals employed by microbes will be critical to the development of new therapeutics.
These continuing discoveries may finally prove once and for all that our fears and anxieties are not actually all in our head. We should attempt to rely more on our gut.
Source: The Conversation
This story is published courtesy of The Conversation (under Creative Commons-Attribution/No derivatives).
![]()