Fighting asthma drug resistance
Current asthma treatments include drugs that open up the tubes of the lungs and corticosteroids that fight lung inflammation. Some patients, however, are stubbornly resistant to corticosteroids, limiting the therapies available to them. Shigeo Koyasu and Kazuyo Moro from the RIKEN Center for Integrative Medical Sciences, in collaboration with Hiroki Kabata of the Keio University School of Medicine and Koichiro Asano of Tokai University and co-workers, have now found that the inflammatory protein called thymic stromal lymphopoietin (TSLP) and its downstream signaling molecules play key roles in the resistance of natural helper (NH) immune cells, a member of group 2 innate lymoid cells (ILC2s), to the anti-inflammatory effects of corticosteroid treatment.
Asthma is a chronic disease of the airways characterized by persistent lung inflammation. The condition is known to be driven by the production of type 2 cytokines, such as interleukin (IL)-5 and IL-13, by NH cells.
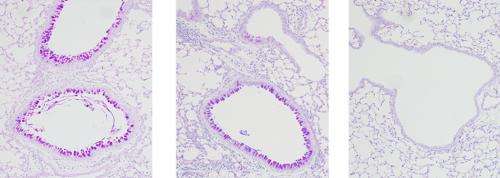
The researchers developed a mouse model for this condition by administering an allergen and the pro-inflammatory cytokine IL-33 to mice. The treatment caused an increase in NH cells and mucus production in the lung, similar to the response observed in the lungs of asthmatic patients. Mice treated with corticosteroids did not show any improvement, indicating that the condition was resistant to the drug.
Koyasu and his colleagues found that the lungs of the mice that received the allergen and IL-33 also had higher levels of TSLP. Separately, they found that the addition of TSLP to NH cells cultured in the presence of IL-33 induced the proliferation of NH cells, even when corticosteroids were present. These findings suggest that TSLP causes NH cells to become resistant to the anti-inflammatory effects of corticosteroid treatment.
In other cell culture experiments the researchers found that in the absence of TSLP, NH cells died more readily under corticosteroid treatment, indicating that an antibody that blocks TSLP could eliminate corticosteroid resistance.
The team then discovered that in the presence of TSLP, NH cells activate the intracellular signaling protein STAT5. Pimozide, widely used as an anti-psychotic drug, is known to inhibit STAT5. Experiments confirmed that pimozide did indeed restore the susceptibility of NH cells to corticosteroids in cell culture (Fig. 1).
The research provides strong evidence that pimozide could be used to eliminate resistance to corticosteroids for the treatment of asthma. "Because pimozide has already been in clinical use for a while, this drug could be applied to patients with corticosteroid-resistant severe asthma after appropriate clinical studies are conducted," explains Koyasu.
More information: Kabata, H., Moro, K., Fukunaga, K., Suzuki, Y., Miyata, J., Masaki, K., Betsuyaku, T., Koyasu, S., & Asano, K. Thymic stromal lymphopoietin induces corticosteroid resistance in natural helper cells during airway inflammation. Nature Communications 4, 2675 (2013). dx.doi.org/10.1038/ncomms3675


















