HIV-infected teens delaying treatment until advanced disease, study shows
Nearly half of HIV-infected teenagers and young adults forego timely treatment, delaying care until their disease has advanced, which puts them at risk for dangerous infections and long-term complications, according to a study led by the Johns Hopkins Children's Center.
The researchers say their findings, published Feb. 3 in JAMA Pediatrics, are particularly troubling in light of mounting evidence that starting treatment as early as possible can go long way toward keeping the virus in check and prevent the cardiovascular, renal and neurological damage characteristic of poorly controlled HIV infection over time. Those most likely to show up in clinic with advanced infections were male and members of a minority group, the study found.
While the researchers did not study specifically why patients were showing up in clinic with advanced infections, they believe some youth were simply unaware of their HIV status, while others had been diagnosed earlier but, for a variety of reasons, did not seek care.
"These are decidedly disappointing findings that underscore the need to develop better ways to diagnose teens sooner and, just as importantly, to get them into care and on therapy sooner," says lead investigator Allison Agwu, M.D., an infectious disease specialist and HIV expert at the Johns Hopkins Children's Center.
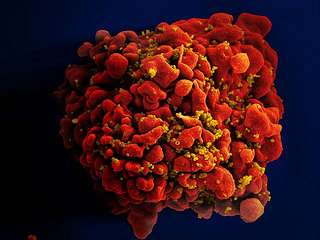
The researchers analyzed records of nearly 1,500 teens and young adults, ages 12 to 24, infected with HIV and seen between 2002 and 2010 in 13 clinics across the country. Between 30 percent and 45 percent of study participants sought treatment when their disease had reached an advanced stage, defined as having fewer than 350 CD4 cells per cubic millimeter of blood. CD4 cells are HIV's favorite target and the immune system's best trained sentinels against infection. Depletion or destruction of CD4 cells makes people vulnerable to a wide range of bacterial, viral and fungal organisms that generally cause no disease in healthy people, but lead to severe life-threatening infections in those with compromised immune systems. In a healthy person, the number of CD4 cells can range between 500 and 1,500 per cubic millimeter. HIV-infected people with CD4 counts below 500 require treatment with highly active anti-retroviral therapy that keeps the virus in check and prevents it from multiplying. Those with CD4 cell counts below 200 have full-blown AIDS.
Even though the U.S. Centers for Disease Control and Prevention recommend HIV testing for everyone between the ages of 13 and 64, many infected people continue to slip through the cracks, the investigators say, due to unwillingness to get tested, fear, stigma and clinicians' biases.
"Clinicians need to get away from their own preconceived notions about who gets infected, stop risk-profiling patients and test across the board," Agwu says.
In addition, Agwu says, pediatricians should help teens view HIV testing as part of their regular physical—just as essential as checking their weight or blood sugar levels.
One finding of particularly grave concern, the investigators note, was that patients with lower CD4 cell counts tended to have more active virus circulating in their blood and bodily fluids, which makes them more likely to spread the infection to others.
Those diagnosed with HIV should start therapy early and be followed vigilantly, the researchers say, to ensure that the virus is under control, to prevent complications and to reduce the risk of spreading the infection to others.
"We have to become more creative in linking those already diagnosed with services so they are not deteriorating out there and infecting others," Agwu says.
Males and members of racial and ethnic minorities were more likely than others to seek care at more advanced disease stages, the study showed. Black youth were more than twice as likely as their white counterparts to show up in clinic at more advanced stages, while Hispanic youth were 1.7 times more likely to do so. Boys and young men were more likely than girls to show up in clinic with lower CD4 cell counts. Males, as a whole, may be at higher risk for delaying treatment, the researchers say, because they tend to receive less regular care than teen girls and young women, whose annual OB/GYN exams make them more likely to get tested and treated sooner.
Males infected through heterosexual intercourse also tended to get to clinic for treatment at more advanced disease stages than homosexual males, a finding that suggests this population may underestimate its own HIV risk. This perception of low risk, the researchers say, may have been fueled inadvertently by public health campaigns that focus on men who have sex with men—the group at highest risk for HIV infection.
"In our study, heterosexual males emerged as this fall-through-the-cracks group," Agwu says. "We've put a lot of emphasis on men who have sex with men in our screening and outreach, but one side effect of this may be that straight males perceive themselves as low risk."
Cindy Voss, M.A., of Johns Hopkins was co-investigator in the research.

















