Newly found tactics in offense-defense struggle with hepatitis C virus
The hepatitis C virus (HCV) has a previously unrecognized tactic to outwit antiviral responses and sustain a long-term infection. It also turns out that some people are genetically equipped with a strong countermeasure to the virus' attempt to weaken the attack on it.
The details of these findings suggest potential targets for treating HCV, according to a research team led by Dr. Ram Savan, assistant professor of immunology at the University of Washington. The study was published in Nature Immunology.
HCV infects more than 150 million of the world's people. The virus is notorious for evading the body's immune system and establishing an infection that can continue for decades, despite treatment. A lasting infection can damage the liver, and in some cases produce liver cancer. HCV infection is a major cause of liver failure requiring an organ transplant.
The virus, hiding in other tissues, can return in the transplanted liver. HCV and the human immune system are engaged in a seemingly never-ending duel, each trying to overcome the others latest move. Several HCV mechanisms for defying the body's immune system have already been uncovered.
Present treatments are about 70 percent effective in curing the infection, Savan said. The triple combination treatments consist of interferon, ribavirin and direct-acting antiviral agents.
He added, however, that resistant strains of HCV are emerging in antiviral treated patients. Also troubling, he said, is that certain patients can undergo almost a year of treatment weeks – and still be infected. They've endured the unpleasant, flu-like side effects of the regimen with little benefit.
After observing that patients of Asian descent reacted better to HCV treatment than did those of African descent, other research teams searched entire human genomes to identify gene clusters associated with response to therapy.
On chromosome 19, the scientists found different, single-letter DNA code changes linked to treatment response and the natural ability to clear HCV infection.
These tiny genetic variations are located near an area that encodes for interferon-lamda3 (IFNL3), also called interleukin-28B. Viruses can trigger blood cells and other cells to produce this potent substance, which is released to protect against virus invasion.
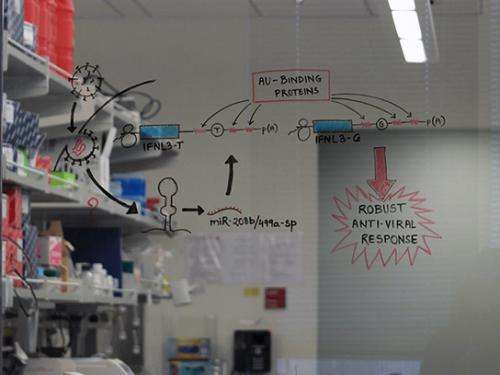
The mechanism aligning this genetic finding with clearance of HCV had been elusive, Savan's group noted in their paper. His team discovered how the single-letter variation in the IFNL3 gene was responsible for the differences between those who could and those who could not effectively clear HCV.
Individuals who carry the T (for thymidine) variant have an unfavorable outcome in fighting HCV, while those who carry the G (for guanosine) variant have a favorable outcome.
Their data showed that HCV could induce liver cells to target the activities of the IFNL3 gene with two microRNAs. MicroRNAs are silencers: They stop the messengers who transmit information to produce a protein from a gene, in this case the production of the antiviral interferon lambda-3.
These two particular microRNAs are generally turned off in liver cells, until HCV coerces them to act on its behalf. Normally, these so called myomiRs are associated with myosin-encoding genes in skeletal and heart muscle.
"This is a previously unknown strategy by which HCV evades the immune system and suggests that these microRNAs could be therapeutic targets for restoring the host antiviral response," the researchers wrote in their paper. Adding support to this suggestion is the researchers' observation that the bad-acting microRNAs in question could not land on and repress interferon lambda-3, if the host carried the favorable "G" variant.
In those cases, the host is able to escape adverse regulation by HCV, the researchers observed. Savan pointed out that this particular escape variant has been found only in humans, and not in other primates. He said it is not yet known if the G variant arose in humans as a response to selective pressure by infection with HCV.
More information: A Nature Immunology News & Views commentary, "Outflanking HCV." by Zhigang Tian of the University Of Life Sciences Of China in Hefei, gives a perspective on the research findings.













