Zero-tolerance approach to MRSA "unachievable", study suggests
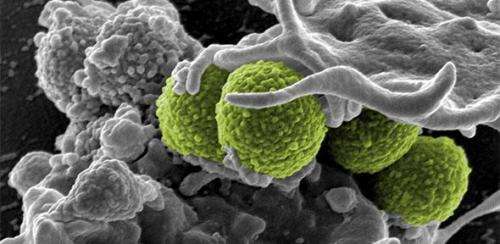
Analysis of a supposed outbreak of MRSA in a Cambridge hospital raises questions about whether the superbug can be completely eradicated, despite a national policy of zero-tolerance.
The zero-tolerance approach to methicillin-resistant Staphylococcus aureus (MRSA) infections in UK hospitals has failed to take account of cases that may be unpreventable, a new study from the University of Cambridge suggests.
The study, carried out by a research team working at Addenbrooke's hospital, Cambridge, investigated a possible outbreak of infections on one of the wards, by sequencing the genomes of MRSA isolated from four affected patients.
The analysis, however, which is published in the Journal of Antimicrobial Chemotherapy, found that the incident was not an outbreak at all. Each of the four patients had a genetically distinct strain of MRSA, and these were highly diverse when compared against a global collection of MRSA samples taken from 15 countries over a period of 20 years.
These findings suggested that, rather than being transmitted between patients on the ward, the MRSA had, in each case, been imported into the hospital by patients, having been acquired elsewhere in the healthcare system.
The researchers argue that this raises serious questions about the feasibility of a long-standing "zero-tolerance" approach to MRSA, which does not take into account the fact that the risk of acquiring it – and of developing subsequent bloodstream infection – varies between different patient populations.
Dr Estée Török, an Academy of Medical Sciences / Health Foundation Clinician Scientist Fellow and Post-Doctoral Researcher at St John's College, Cambridge, was the study's lead author. She said: "Since the late 1990s, successive governments have talked about a zero-tolerance approach to MRSA. This was originally a policy applied to fighting small-scale crime in America. To apply it to the health service is a flawed concept, but in spite of that, it is now becoming an established view."
"We should absolutely be aiming to get MRSA rates as low as we can, but there is little point in setting a standard which is unachievable without unrealistic levels of investment."
Reducing hospital-based MRSA bloodstream infections is a national healthcare priority and has met with considerable success in recent years. Between 2001/2 and 2012/13, there was an 87% reduction in the number of cases reported to Public Health England. This followed the introduction of a range of infection control measures, which were mandated by the Department of Health. Hospitals are set annual limits for MRSA bloodstream infections and those that overshoot their targets can incur severe financial penalties.
While the overall rate of MRSA bloodstream infections at Addenbrooke's have fallen in line with the national trend, the new study examines a suspected outbreak which occurred between September 2011 and August 2012, when four patients on its specialist liver unit were diagnosed with the bug. Routine lab tests suggested that the type of MRSA in each case was the same, indicating a possible outbreak.
The researchers took blood from each patient, isolated the MRSA, and sequenced the entire genome of each bug. This more detailed analysis revealed that the strains were in fact completely different. "The diversity of the variants was so wide that it could have been a random sample from the whole of the UK population," Török added.
To confirm their findings, the researchers identified 42 other patients who were found to be MRSA positive for the first time, and who had been admitted to the liver unit during the previous 12 months. Samples from these patients were sequenced, and compared against 193 MRSA isolates from a global collection of isolates from 15 countries, gathered between 1990 and 2009.
These samples, including the four from the supposed outbreak, were shown to be scattered throughout the global picture in terms of their genetic diversity. Such diversity would not have been consistent with a ward-based outbreak, in which a strain would be passed from patient to patient. Instead, it suggested that most individuals had imported their own specific strain of MRSA from outside the hospital.
Each of the four patients had been screened for MRSA and had received standard treatment for MRSA carriage, but this had not prevented them from developing a bloodstream infection. The severity of their underlying liver disease meant that they were already extremely vulnerable to developing MRSA infection, either as a result of broken skin, or through the use of intravenous catheters which were necessary for their care.
"Overall, we have very robust systems in place for MRSA control, but specialist wards dealing with complex patients will not always be able to completely eradicate it," Török said. "The study shows that infections sometimes happen in circumstances which may not be preventable, and that means that the application of terms such as zero-tolerance is inappropriate. The imposition of punitive financial penalties for exceeding targets for healthcare-associated infections in this context is unlikely to improve infection control practices, and nor is it likely to benefit patients."
Dr Nick Brown, Consultant Medical Microbiologist at Addenbrooke's Hospital, said: "This study reiterates the importance of genome sequencing in infection control to understand how infections spread between people. This helps hospitals, GPs and other healthcare providers to effectively plan and target resources. At Addenbrooke's our key priority is to prevent all avoidable infections and this is supported by our cleaning, hygiene and hand-washing practices. We have successfully brought down the numbers of serious MRSA infections from over 126 per year to a handful of cases in less than a decade. This reflects that commitment of our staff and indicates that the measures we have put into place are working."
More information: Zero tolerance for healthcare-associated MRSA bacteraemia: is it realistic? M. Estée Török, et al. Antimicrob. Chemother. (2014) 69 (8): 2238-2245. DOI: 10.1093/jac/dku128 . First published online: April 30, 2014.















