New device diagnoses sick people using a mobile phone and the cloud

Remote diagnostics is an emerging field that allows healthcare workers to perform tests on patient samples in the field and to get results interpreted by medical experts remotely. This is a groundbreaking approach to providing affordable healthcare to patients in some of the world's poorest countries.
Providing healthcare in this way, though, often means using expensive equipment, supplying extensive training and getting access to relatively developed telecommunications infrastructure. In a paper published in the Proceedings of the National Academy of Sciences today, we present a device that has the potential to overcome these challenges.
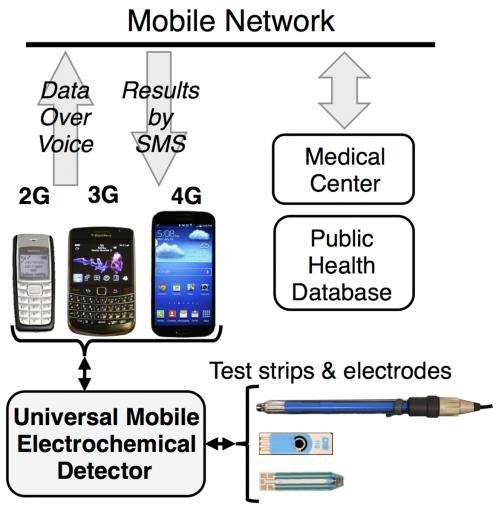
Costing only US$25, the universal Mobile Electrochemical Detector, or uMED, can perform chemical and biochemical tests on a variety of commercially available test strips and electrodes and send the results over an audio cable connected to the headphone jack of any cell phone – even if it isn't a smartphone. After placing a phone call, the user can upload the data over the voice channel of any mobile network (2G, 3G, or 4G) that is present on site. There is no need for an internet connection.
An automated cloud database or a medical expert can then return relevant information about test results to the device by text message. The cloud database might be run by a private hospital or a government agency, which can send help if needed. On the other side, that agency can track the results uploaded through uMED to keep tabs on the spread of a disease.
The uMED can be used to test for toxic metals in drinking water, to measure a patient's blood-glucose and electrolyte levels, and even to quantify and diagnose malaria. It could also be used in the future to screen for other diseases, such as Ebola, HIV, E. Coli, hepatitis, influenza, West Nile virus or Dengue fever.
There are already various low-cost devices that can be used to test patients' health or to diagnose certain diseases. Pregnancy tests, blood-glucose tests and rapid malaria tests all have their uses but are often too limited in what they can detect. In general, diagnostic tests can be either versatile and accurate but expensive and complicated, or rapid and cheap but limited and insensitive. We believe our approach fuses the strengths of these technological extremes, and avoids their weaknesses.
How it works
Electrochemical detection is widely used to perform chemical testing in well-resourced laboratories. In this type of testing, a voltage applied to a chemical sample causes a reaction that yields a detectable flow of current. The reaction can be controlled to ensure the current produced is related to the concentration of the chemical sample. In this way, concentrations of various chemicals can be measured by interrogating the samples with electronics.
Apart from blood-glucose metres, though, these types of measurements typically need expensive and sophisticated instruments. We redesigned a laboratory electrochemical analyser from the ground up to be affordable and tailored it to specifically measure fluid samples with physiological concentrations. It was important to us that all these sophisticated functions could be offered in a single, automated, hand-held device that resembled a blood-glucose meter, because this device in particular is familiar to a lot of people around the world.
To build the uMED, we developed a custom electrochemical sensor compatible with the open-source development environment Arduino. This means the uMED can be easily adapted to local needs, and reprogrammed or updated with minimal training. We also added a vibration motor, similar to those found on cellphones, to mix samples when necessary. This eliminated the need for addition equipment that is typically necessary to stir samples during measurements.

Although the use of smartphones is rapidly rising, there remain almost three billion people in the world today who still use older technologies for communication, and according to market trends, that number is not set to decrease much over the next decade. That's why we needed to make uMED compatible with even low-end phones. There is huge potential to improve the health of people and animals in countries where mobile phones are everywhere but high-tech infrastructure is not.
For most tests, all a healthcare worker needs to do is insert a strip containing a blood, urine, or water sample (or dip an electrode into the sample), select the test they want to perform, and make a phone call to send the results. These can be glucose test strips, screen-printed electrodes, ion-selective electrodes or ultra-low-cost, paper-based electrodes.
The uMED is still a work in progress, and we're working with devices firm Diagnostics For All to improve its diagnostic capacity, particularly in difficult environments. Field trials will start in India soon, with the hope of moving towards a device that can make healthcare easier, even before the internet arrives in hard-to-reach areas.
This story is published courtesy of The Conversation (under Creative Commons-Attribution/No derivatives).
![]()




















