Experts question value of common superbug control practices
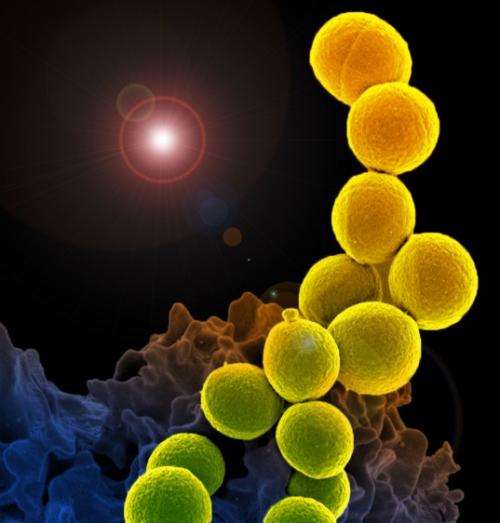
The jury is still out on the effectiveness of meticillin-resistant Staphylococcus aureus (MRSA) superbug control policies in hospitals, according to leading infectious disease experts in a Viewpoint published in The Lancet. In particular, screening and isolating infected patients—which have long been regarded as the gold standard MRSA prevention strategy and are required by law in some countries—have poor evidence for their effectiveness, say the authors.
After reviewing studies on preventing the spread of MRSA in hospitals over the past decade, the authors argue that although various approaches to tackle MRSA have been examined, most of the research has looked at bundles of control measures, and we don't yet know which individual components work best, or whether some of them could be omitted without increasing transmission.
Gerd Fätkenheuer, study co-author and Professor of Infectious Diseases at the University Hospital Cologne in Germany and President of the German Society of Infectious Diseases explains, "In the haste to do something against the rising tide of MRSA infection, measures were adopted that seemed plausible but were not properly assessed, bundling the effective and harmless with the ineffective and harmful. We know, for example, that isolating patients can result in anxiety and depression and fewer visits by doctors and nurses."
"We need better studies", says co-author Professor Bernard Hirschel, former Chief of the HIV unit at the Geneva University Hospitals in Switzerland and current President of the Swiss Society of Infectious Diseases. "With the tide of MRSA receding and improved treatment options for the infection, a window of opportunity now exists to reassess whether masks, gowns, gloves, and single rooms add anything to the traditional infection control measures of hand hygiene and universal decolonisation (eg, a daily bath with an antibacterial agent) which have proved much more successful in reducing rates of MRSA."
In recent years, MRSA rates have declined and hospitals are facing multiple multidrug resistant pathogens. The key question now, say the authors, is whether scarce resources should focus on screening for one particular pathogen, or assume a broader approach focusing on reducing all hospital-acquired infections, not just MRSA.
According to co-author Professor Stephan Harbarth from Geneva University Hospitals in Switzerland, "The lack of effectiveness of active detection and isolation should prompt hospitals to discontinue the practice for controlling the spread of MRSA in favour of evidence-based measures adapted to local conditions and settings, which weigh up effectiveness, costs, and adverse events. What is more, recommendations and guidelines should clearly state the uncertainties in this field, and legal mandates that dictate the use of specific control measures for MRSA should be abandoned."
More information: The Lancet, www.thelancet.com/journals/lan … (14)60660-7/abstract















