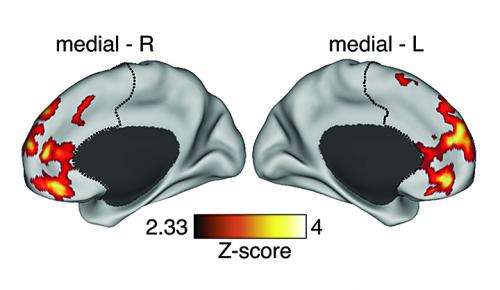
Colored areas represent areas of heightened brain cell connectivity in prefrontal cortex of freshly diagnosed schizophrenia patients. Credit: Michael Helfenbein
In its chronic stage, schizophrenia is typically marked by a dearth of links between brain cells in the prefrontal cortex, the region of the brain responsible for higher-order thinking. However, a new study by Yale and Chinese researchers shows that the onset of the disease—usually in the early 20s—is marked by an abnormal spike in neural connections.
The surprising finding, published in the Jan. 7 issue of The journal Neuroscience, suggests new strategies for treatment during early stages of the illness that afflicts 20 million people worldwide with debilitating delusions, hallucinations, disorganized thinking, and cognitive deficits.
"After the first episode at least, it appears that is not the lack of brain signals that produces abnormal internal states in schizophrenia but instead excessive communication," said Alan Anticevic, assistant professor of psychiatry and lead author on the paper.
Most schizophrenia research focuses on individuals who have been afflicted for many years. The Yale team, in conjunction with colleagues at the Huaxi Magnetic Resonance Research Center at Sichuan University in China, analyzed fMRI data from 129 unmedicated individuals who had recently experienced their first psychotic episode but had not yet undergone treatment.
As predicted by a sophisticated mathematical model developed with researchers at New York University, the Yale team found that when compared to healthy controls newly diagnosed schizophrenia patients had heightened connectivity in the prefrontal cortex relative to a healthy comparison group. Intriguingly, note the researchers, this "hyper-connectivity" subsided in those subjects who were studied and received treatment over the following year. The patients also showed a decrease in psychotic symptoms.
Anticevic cautioned it is unclear whether the excess of connectivity causes symptoms of schizophrenia or whether this neural "signature" is the result of some other process, such as fever is a response to infection. If further research establishes this link then individuals during early-stage schizophrenia might benefit from drugs that can minimize the abnormal spike in neural communication, notes Anticevic.
His lab is also studying why individuals with chronic schizophrenia exhibit cognitive and neural deficits in later stages of the disease and how they may differ from those during incipient stages of the illness. He notes that during late teen years, a heightened period of risk for psychosis, the brains of young adults are pruning unneeded synaptic connections. He speculated that an initial failure in this process could set off a cascade of events that unmask neurodevelopmental abnormalities that had been present since birth.
Journal information: Neuroscience
Provided by Yale University