As glaucoma cases soar, researchers focus on solutions

Ernest Murry saw glaucoma steal his mother's vision, just as it had robbed sight from many other family members. There was a time when it seemed the same might happen to him. "When I went outside to walk, I would have to pat in front of me to keep from falling," he says.
After several surgeries and intensive treatment from physicians in the UAB Callahan Eye Hospital Clinic, Murry's vision loss has been arrested. "Now I'm doing wonderful," says the 68-year-old Bessemer resident. "I have my own apartment and can do for myself."
Advances in glaucoma therapies, including powerful eye drops and minimally invasive laser surgeries, mean few patients today would lose their vision if they were treated in time. But "many people don't notice they are losing vision until it's too late," says Murry's physician, Lindsay Rhodes, M.D., an assistant professor in the UAB Department of Ophthalmology. "Glaucoma is a disease that affects the optic nerve, which connects the eye to the brain," Rhodes explains. The nerve deteriorates over decades, starting at the periphery of sight and slowly severing the eye-brain link.
There is no way to reverse this deterioration. "That's the hardest part about glaucoma, and something we always emphasize with patients," Rhodes says. "We can never recover what they've lost. The goal of treatment is to not lose more."
Race Against Time
Despite more than a century of research, the underlying causes of the nerve damage in glaucoma are still a mystery. So is the strong racial disparity to the disease: People of African descent, such as Murry, are up to five times more likely to suffer from glaucoma than people of European descent. But a major research effort from the Department of Ophthalmology is uncovering intriguing new clues to these riddles. Using high-tech devices and innovative outreach programs, UAB teams are pioneering fresh approaches to an age-old problem of old age.
Aging, in fact, is the strongest risk factor for glaucoma, which puts researchers and clinicians in a race against time. Glaucoma currently affects some 2.7 million Americans, according to the National Eye Institute, but that number is expected to double by 2050 as the baby boom generation goes gray.
The problem is particularly acute in Alabama, says Christopher Girkin, M.D., chair of the Department of Ophthalmology. Girkin founded the UAB Glaucoma Service in 1999; today, the program has grown to include seven glaucoma specialists and an international team of researchers. UAB is already one of the country's busiest glaucoma centers, Girkin says, and patient volumes are expected to more than double in the next decade.
"Having a large team of subspecialists focused on glaucoma allows for a unique interchange of perspectives vital to the optimization of care for our patients," Girkin says. "The breadth of expertise allows us to provide a unique complement of diagnostic and therapeutic methods, including cutting-edge minimally invasive and experimental procedures."
Power to the People
Much of the department's clinical research in glaucoma "is looking at new imaging methods and tests that allow us to detect the disease earlier," says Girkin. But it is also important, he notes, to "get this technology out into the community," especially to underserved areas and patient populations.
In 2013, the department launched a novel telemedicine approach to do just that. The EQUALITY trial, funded by a $1.9-million grant from the Centers for Disease Control and Prevention, has installed sophisticated optical coherence tomography machines in the offices of independent optometrists located adjacent to two Walmart Vision Care Centers in central Alabama.
The machines capture high-resolution images of a patient's eyes and transmit those images to UAB for analysis by glaucoma specialists. If patients are diagnosed with glaucoma, then the UAB physicians collaborate with the local optometrists to determine the most appropriate treatment plan.
"People have to get their eyes checked several times a year, and all the specialists are in Birmingham," Rhodes says. "If we can develop ways to check eye pressure and do this imaging remotely, then we can reach people before they start losing their vision, and we can keep a closer watch on patients and keep them from getting worse."
Pressure and Race
The primary focus of diagnostic exams, and follow-up testing, is intraocular pressure, or the fluid pressure inside the eye. Rising pressures indicate that the disease is getting worse, and all current glaucoma treatments work by reducing intraocular pressure. The trouble is, intraocular pressure isn't always a reliable indicator of a person's risk.
"Many patients with high pressure never get glaucoma, and others with 'normal' pressure do get the disease," Girkin says. That means that some patients don't need the expensive eye drops that are the front-line treatment for high intraocular pressure, while others need aggressive treatment, even though their pressures are normal. "One key area of our research, both on the clinical and the basic side, is trying to figure out new treatment options to halt glaucoma progression beyond lowering of eye pressure," says Girkin.
Girkin's own research is "focused on health disparities, and in particular why African-Americans are at greater risk for glaucoma," he says. Health-care access and socioeconomic factors play a major role, Girkin notes, but research at UAB and elsewhere has shown that there are definite "racial differences in the structure of the optic nerve head"—the point at which the optic nerve exits the eye. Defining these anatomic weak points will help all patients, Girkin points out, because they can be present in all races, even though they are more prevalent in people of African descent.
Eyes, Reconstructed
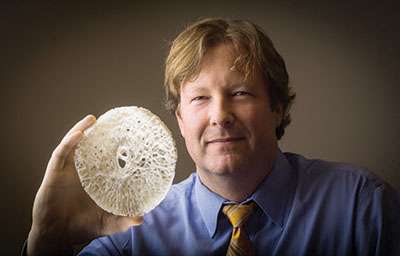
To expand UAB's research efforts in this area, Girkin recruited longtime collaborator J. Crawford Downs, Ph.D., an internationally renowned glaucoma researcher at the Devers Eye Institute in Oregon, to launch the UAB Ocular Biomechanics and Biotransport Program in 2012. Downs was one of the first scientists to take a biomechanics approach to the eye—using engineering principles to model the organ's complexity and analyze weak points in its design. It's the same approach an aerospace engineer would take to find flaws in a jet, Downs explains, "except the eye is much more complex than the wing of a 747."
Downs is particularly interested in a part of the optic nerve head known as the lamina cribrosa. This crucial structure, barely wider than a pencil lead, acts as a mechanical seal around the optic nerve as it passes out of the eye on its way to the brain. "It's the place where the nerves get damaged in glaucoma," Downs says. "We want to understand the mechanics of that structure and what it looks like in three dimensions."
To do that, Downs invented and built a "fluorescent three-dimensional histologic reconstruction device." The fully automated machine takes a section of tissue from a human donor eye and slices it into thousands of pieces, snapping a photo of each slice. These images are combined to generate a high-resolution, three-dimensional model of the donor's lamina cribrosa at a volumetric resolution some five million times better than the most advanced MRI. "Once we get that, we can put it in a computer, apply pressure to it, and see what happens," Downs says.
By comparing models from patients of different races and ages, the researchers are already discovering new insights about the factors that make some patients more likely to suffer nerve damage, even at lower intraocular pressures.
Laser Vision
Downs isn't the only inventor in UAB's Department of Ophthalmology. Assistant professor Massimo Fazio, Ph.D., has built a unique, ultra-precise device to track the eye's response to pressure. Fazio created the machine with his former doctoral advisors from the University of Calabria in Italy, Luigi Bruno, Ph.D., and Andrea Poggialini, Prof. It focuses four laser beams on a donor eye, which is immersed in a saline bath and can be inflated to simulate a range of eye pressures. One beam arrives slightly after the others, allowing the researchers to measure—at nanometric precision—the tiny, fleeting mechanical changes in the shape of the eye as it responds to changes in intraocular pressure. Four synchronized high-speed cameras record the data at 150 images per second.
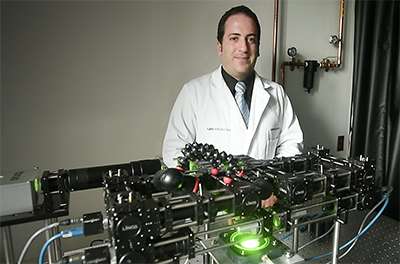
Downs's recent investigations have shown that each time we blink or move the eye, a wave of pressure rolls through the eye within a few milliseconds, forcing it to expand like a rubber ball. The effects of these rapid shifts in intraocular pressure have never been fully explored in the past, because scientists had not developed the right technology. With his laser device, Fazio is now doing those studies on donor eyes from patients of different ages and races. "We are concerned that this pressure impulse is transferred to the posterior pole of the eye, and possibly to the optic nerve head," he says. "Understanding the eye's response to these highly variable mechanical events might be very important to understand what's causing glaucoma—and eventually how to address and prevent it."
"We know that these pressure spikes get bigger as you age, because your eye gets stiffer, like all your other joints, so the eye can't expand as much," Downs adds. "That could be important, or it might not be. Right now, we're trying to figure out the most important factors to measure in order to expand our knowledge of glaucoma."
Translational Success
The ultimate goal of all of this research, Downs says, is to develop a test that can identify patients at highest risk for glaucoma years before the disease begins to cause problems. "That's the holy grail," he says. "Glaucoma is very expensive to treat, and we have to treat many more people than need to be treated, because we don't know who will go on to develop glaucoma and who won't."
UAB's strengths in basic research and clinical care for glaucoma create powerful synergies, Girkin notes. "We can enroll patients in clinical studies and follow them over time, and then look back at imaging and function testing and figure out the risk factors associated with progression," he says. "We can correlate what we see in the lab with what's going on in the clinic."
Girkin says the department's strategic investment in glaucoma research will continue to grow, buoyed by philanthropic support. He is now recruiting a world-class investigator to hold the new Dennis-McKee Endowed Chair in Glaucoma Research. "Our goal is to make significant breakthroughs in the understanding of glaucoma that will move us closer to eliminating the suffering caused by this disease," he says.
Catching the Silent Thief
Glaucoma is known as the "silent thief of sight" because symptoms appear so slowly that many people don't realize anything is wrong until they have permanent damage.
The Glaucoma Foundation recommends that everyone under age 40 should have a comprehensive eye exam every three to four years. Those 40 and older should get a comprehensive exam every one-and-a-half to two years. So should anyone under 40 with one of these important risk factors:
- a family history of glaucoma;
- African, Latino, or Asian heritage;
- diabetes; or
- extremely high or low blood pressure.
















