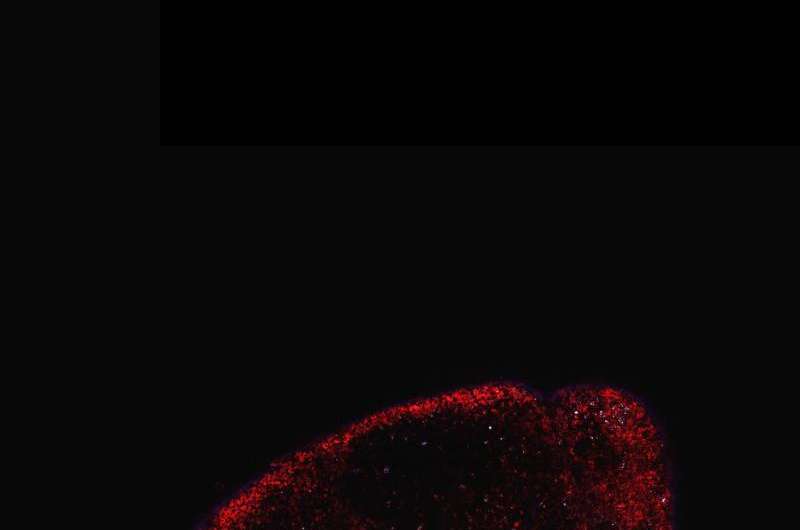
Credit: PNAS, 10.1073/pnas.1502609112
A novel approach that allows real-time imaging of the immune system's response to the presence of tumors—without the need for blood draws or invasive biopsies—offers a potential breakthrough both in diagnostics and in the ability to monitor efficacy of cancer therapies.
The method, developed in the lab of Whitehead Institute Member Hidde Ploegh and reported online this week in the Proceedings of the National Academy of Sciences (PNAS), harnesses the imaging power of positron emission tomography (PET), which is normally used to monitor cancer metabolism, to identify areas of immune cell activity associated with inflammation or tumor development.
"Every experimental immunologist wants to monitor an ongoing immune response, but what are the options?" Ploegh asks rhetorically. "One can look at blood, but blood is a vehicle of transport for immune cells and is not where immune responses occur. Surgical biopsies are invasive and non-random, so, for example, a fine-needle aspirate of a tumor could miss a significant feature of that condition."
In search of a better monitoring approach Ploegh leveraged two research tools that have become staples in his lab in recent years. The first exploits so-called single-domain antibodies known as VHHs, derived from the heavy chain-only antibodies made by the immune systems of animals in the camelid family. Ploegh's lab immunizes alpacas—his camelid of choice—to generate VHHs specific to immune cells of interest. The second tool, known as sortagging, labels the VHHs in site-specific fashion to enable the tracking of the VHHs and their targets in a living animal.
Knowing that the tissue around tumors often contains immune cells such as neutrophils and macrophages, Ploegh and his lab members hypothesized that appropriately labeled VHHs might allow them to pinpoint tumor locations by finding the tumor-associated immune cells. Ploegh notes that VHHs' extremely small size—approximately one-tenth that of conventional antibodies—are likely responsible for their superior tissue penetration and thus makes them particularly well suited for such use.
For the current research, the lab generated VHHs that recognize mouse immune cells, then labeled these VHHs with radioisotopes, and injected them into tumor-bearing mice. Subsequent PET imaging detected the location of immune cells around the tumor quickly and accurately.
"We were able to image tumors as small as one millimeter in size and within just a few days of their starting to grow," says Mohammad Rashidian, a postdoctoral researcher in Ploegh's lab and first author of the PNAS paper. "We're very excited about this because it's a powerful approach to pick up inflammation in and around the tumor."
Rashidian and Ploegh believe that with further refinement, the method could be used to monitor response to—and perhaps modify—cancer immunotherapy, which, though quite promising, has thus far met with great success in some cases, but has failed in others.
"To succeed with immunotherapy, we need more information about the tumor microenvironment," says Rashidian. "With this method, you could perhaps start immunotherapy, and then, a few weeks later, image with VHHs to figure out progress and success of treatment."
Adds Ploegh: "PET imaging should allow a much more comprehensive look at the entire tumor in its environment. Then we can ask, 'Did the tumor grow? Did immune cells invade? What has happened to the tumor?' And to be able to see this without going in invasively is a significant achievement."
More information: "Noninvasive imaging of immune response" PNAS, April 20, 2015 (online): www.pnas.org/cgi/doi/10.1073/pnas.1502609112
Journal information: Proceedings of the National Academy of Sciences
Provided by Whitehead Institute for Biomedical Research