Study discovers how pancreatic cancer spreads to the liver
An international team led by Weill Cornell Medical College investigators has illuminated the precise molecular steps that enable pancreatic cancer to spread to the liver—the event that makes the most common form of the disease lethal. By understanding this process, investigators say their discovery can lead to targeted treatments that delay metastasis, and could offer clinicians a new biomarker to test for the earliest signs of pancreatic cancer.
The study, published May 18 in Nature Cell Biology, focuses on the role of small, spherical tumor-secreted packages, called exosomes, which contain tumor-derived proteins, in preparing a liver microenvironment fertile for pancreatic cancer metastasis.
Nearly 49,000 people in the United States will be diagnosed with pancreatic cancer, and more than 40,000 of them will succumb to it, according to estimates from the American Cancer Society. Pancreatic cancers are among the most lethal cancers—only six percent of patients survive five years after diagnosis, with the median survival rate being just six months.
"What makes this cancer so lethal is that patients don't generally become symptomatic—and as such aren't diagnosed—until the cancer is very advanced and treatment options are limited," said senior author Dr. David Lyden, the Stavros S. Niarchos Professor in Pediatric Cardiology and a professor of pediatrics in the Department of Pediatrics at Weill Cornell Medical College.
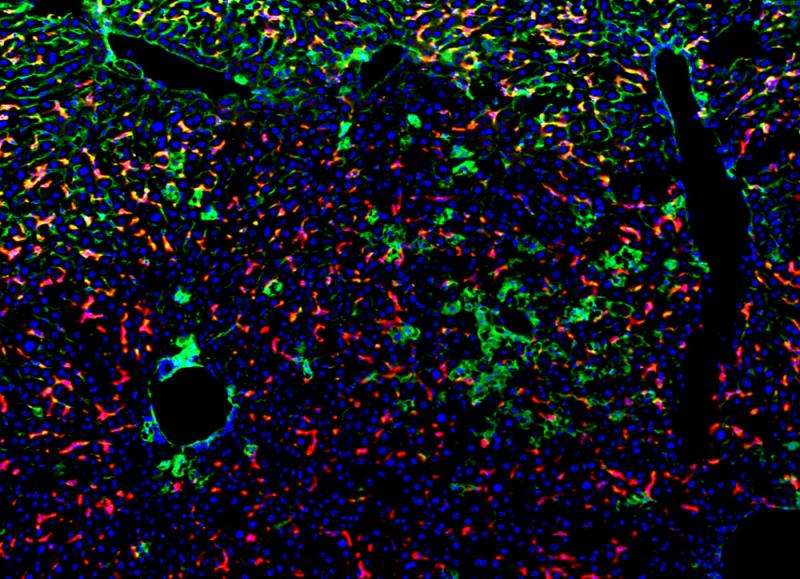
In the study, the investigators recreated the environment for pancreatic cancer using mouse models and discovered that exosomes were finding their way to the liver during the cancer's earliest stages. Once in the liver, the exosomes were taken up by resident immune cells, called Kupffer cells. This process changed the Kupffer cells' gene expression and protein composition, and educated them to produce a powerful protein. This protein, in turn, affected the behavior of a group of cells, inducing liver fibrosis. Liver fibrosis is an overly exuberant wound healing process that can interfere with normal liver function, and creates a microenvironment auspicious for tumor seeding and growth.
When investigating how exosomes exerted these effects on liver cells, Dr. Lyden and his team found that pancreatic cancer exosomes contain a protein called macrophage migration inhibitory factor (MIF). When the investigators eliminated MIF from exosomes, they noticed that they had prevented the creation of a fibrotic, tumor-supporting environment in the liver.
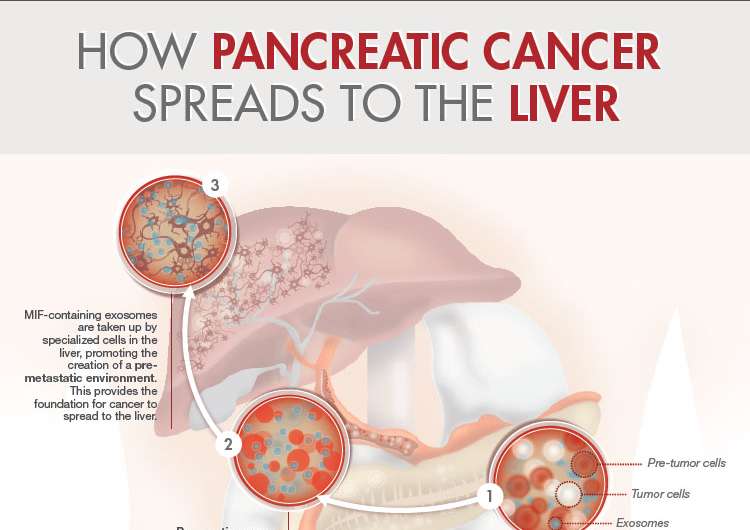
"In mouse models of pancreatic cancer progression, exosomes containing MIF are released in circulation prior to the onset of a recognized pancreatic carcinoma and can 'educate' the liver, inducing fibrosis," said first authorDr. Bruno Costa Silva, an instructor of cell and developmental biology in pediatrics at Weill Cornell. "Our findings suggest that a microenvironment ripe for metastasis is generated at an earlier stage of the disease than previously recognized."
Once they understood this process, the investigators attempted to block each individual step in this sequence."Disrupting just one part of the process at any point of the circuit decreased metastasis, a discovery that could lead to the development of multi-targeted therapies that could prolong patients' lives," said Dr. Lyden, who also has appointments in the Sandra and Edward Meyer Cancer Center and the Gale and Ira Drukier Institute for Children's Health. Dr. Lyden and his team conduct their research in the Children's Cancer and Blood Foundation labs at Weill Cornell.
Dr. Lyden and his team also found that MIF is highly expressed in exosomes circulating in patients who have advanced pancreatic cancer. When they examined pancreatic cancer blood samples, the scientists discovered that exosomal MIF was much higher in patients who went on to develop liver metastasis than in those who escaped it. They say this protein signature could be used to predict which patients would then go on to develop liver metastatic disease. These discoveries were made possible by an international collaboration between researchers at Weill Cornell Medical College, Memorial Sloan Kettering Cancer Center, University of Nebraska Medical Center, University of Pennsylvania and Oslo University Hospital.
Since five percent of patients diagnosed with pancreatitis—a disease characterized by inflammation—go on to develop pancreatic cancer, the investigators believe MIF could also serve as a biomarker for clinicians to monitor disease progression. Dr. Lyden and his team are currently testing whether measuring MIF levels in exosomes isolated from patients' blood can accurately estimate the risk of pancreatic cancer in patients with non-malignant pancreatic lesions. This type of "liquid biopsy" could allow the clinicians to initiate treatments, such as surgical resection, earlier in patients at risk, preventing disease progression.
More information: Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver, DOI: 10.1038/ncb3169


















