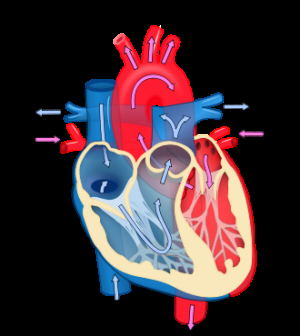
Heart diagram. Credit: Wikipedia
A higher resting heart rate and lower heart rate variability in older adults at high risk of heart disease are associated with poorer ability to function in daily life as well as future decline, according to a new research in CMAJ (Canadian Medical Association Journal).
"It has been hypothesized that heart rate and heart rate variability are markers of frailty, an increased vulnerability to stressors and functional decline," writes Dr. Behnam Sabayan, Department of Gerontology and Geriatrics, Leiden University Medical Center, Leiden, the Netherlands, with coauthors. "However, the direct link between these 2 parameters and risk of functional decline has not been fully established."
Heart rate variability is the beat-to-beat variation in heart rate intervals. Heart rate and heart rate variability mirror the adaptability of the heart to stressors.
To determine whether heart rate and heart rate variability were correlated with functional status—that is, the ability to perform daily living activities—a team of European researchers looked at data on 5804 people aged 70 to 82 years with risk factors for heart disease from Ireland, Scotland and the Netherlands. Just over half (52%) were women. The researchers measured the Barthel Index of activities of daily living (ADL), which includes grooming, toilet habits, walking and more, and the Lawton Instrumental Activities of Daily Living Scale (IADL), which measures more complicated tasks, such as taking medications as prescribed, doing housework, shopping and others.
"Because functional disability develops gradually, it is important to identify it early and take steps to delay decline, such as exercise, medication and other interventions," states Dr. Sabayan. "This is especially important with an ageing population, which could mean rising numbers of people who have problems with daily functioning."
The researchers followed the participants on average for 3.2 years and found that people with the highest resting heart rate had an almost 80% increased risk of decline in performing basic activities on the ADL scale. They also had a 35% increased risk of decline in performing the more complex IADL tasks. People with the lowest heart rate variability had approximately a 25% increased risk of decline in performing both ADL and IADL tasks.
"Higher resting heart rate and lower heart rate variability were associated with worse functional performance at baseline and with higher risk of future functional decline in older adults at high cardiovascular risk," conclude the authors.
The study is consistent with previous studies and expands the evidence by showing that the association of heart rate and heart rate variability with functional decline is the same in men and women.
More information: CMAJ, www.cmaj.ca/lookup/doi/10.1503/cmaj.150462
Journal information: Canadian Medical Association Journal
Provided by Canadian Medical Association Journal