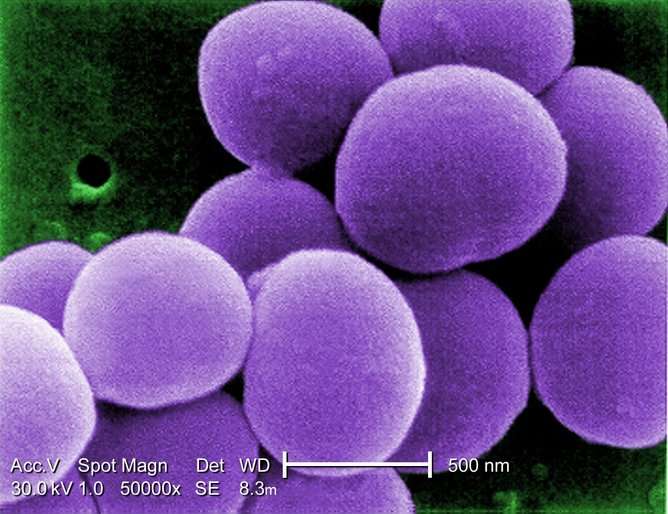
Staphylococcus aureus has confused researchers about how superbugs cause deadly infections. Credit: Janice Haney Carr/wikimedia
Infamous bacteria such as MRSA are considered "superbugs" because not only can they kill us using a wide range of virulence mechanisms, but they can also resist the effects of antibiotics. However, some superbugs reside on the skin and in the noses of a huge proportion of the human population causing only negligible problems for the majority.
Exactly why certain bacteria cause more severe infections than others is unclear. But for decades we have believed that the more toxins a bacteria produces, the worse infections it causes.
However, our latest study shows that, in the case of the bacterium Staphylococcus aureus (the SA in MRSA but also known as "golden staph"), quite the opposite is true.
The role of toxins
It is vitally important that we understand the link between superbugs and infections in detail. While infections due to S. aureus residing in the nose and skin can be mild and superficial, they can be life-threatening if they get in the bloodstream. Blood is normally a sterile environment, but bacteria can occasionally enter it during surgery or complications due to infections like pneumonia or other underlying health conditions such as diabetes. This serious condition, called bacteraemia, has mortality rates as high as 40%.
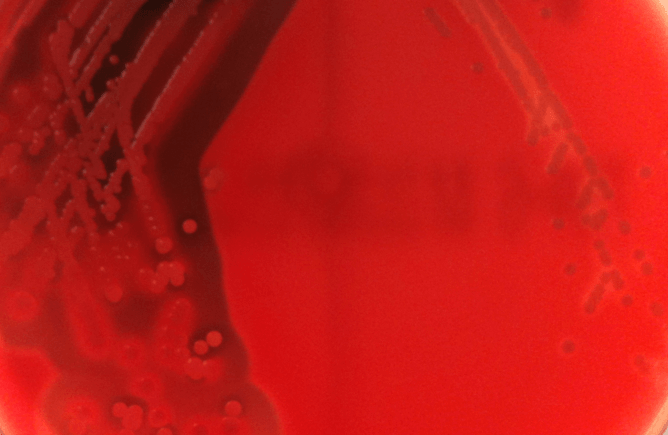
To try to understand this difference in severity, we focused on the ability of these bacteria to secrete toxins: proteins that physically destroy the membrane of human cells. The effect of bacteria-producing toxins on blood cells can be seen in the figure below. On the left we have highly toxic bacteria growing and a halo of broken-down blood cells can be seen, whereas on the right non-toxic bacteria are growing and the blood cells remain intact.
High and low toxic MRSA growing on the surface of horse-blood agar plates.
Given the destructive nature of bacterial toxins, we have for decades believed that the more toxic a bacteria is, the worse the severity of infection it can cause. To study this we examined two large collections of isolated S. aureus bacteria. One was from a patient before and after they developed bacteraemia. The second was from a wide range of patients, some isolated from their noses and some from their bloodstream after they developed bacteraemia.
Surprisingly, we found that in both cases, the bacteria from the bloodstream, which cause the most severe disease, were the least toxic. We also discovered that the fitness of the bacteria is key to this effect. Secreting toxins expends high levels of energy by the bacteria. And the bloodstream, where the majority of the human immune system exists primed and ready to respond to invasion, is a highly stressful environment for it.
We therefore believe that the energy required to produce toxins is too high for the bacteria to be able to also adapt to the high-stress environment of the bloodstream. This is why the less toxic bacteria get in there, causing the most severe of infections.
Challenging the dogma
This leaves us with the question of why we have for decades believed toxins to be so critical for bacteria to cause disease, to the extent that they have been the focus of numerous research labs across the globe and one of the major protein targets for vaccination programmes. Unfortunately, it's a question to which there is no simple answer.
Toxins are important to many aspect of S. aureus' life style. They kill off competitor bacteria, they release nutrients from human cells, they dampen down the human immune system allowing the bacteria to reside happily on our bodies as part of our normal flora. When they cause minor infections toxins are responsible for producing lots of pus, which is a great material for transmitting from one person to another … after all, who can resist popping a pimple?
But as there is no way to mimic all the complex interactions that occur in the body for serious bacterial infections, we are reliant on animal models to try to understand them. For S. aureus these are typically small rodents who do not naturally succumb to this pathogen. As such 10-100 million bacterial cells need to be injected directly into the rodent's bloodstream to get experimentally reproducible infections. Compare this to the small handful of bacteria required to cause such infection in humans (<100) and it is clear to see where misinterpretations of such research findings can occur.
At a superficial level, the implications of our research are somewhat depressing in that despite decades of research we still have much to learn about how bacteria such as MRSA cause life-threatening disease. However, identifying the limitations to our knowledge, rather than blindly pursuing hypothesis based on misleading animal experiments has got to be a better starting point for the future of infectious disease research.
Source: The Conversation
This story is published courtesy of The Conversation (under Creative Commons-Attribution/No derivatives).
![]()