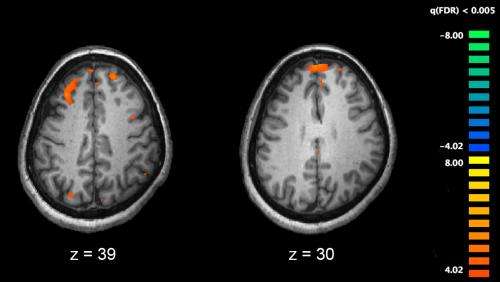
Functional magnetic resonance imaging (fMRI) and other brain imaging technologies allow for the study of differences in brain activity in people diagnosed with schizophrenia. The image shows two levels of the brain, with areas that were more active in healthy controls than in schizophrenia patients shown in orange, during an fMRI study of working memory. Credit: Kim J, Matthews NL, Park S./PLoS One.
A novel research tool developed by researchers from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King's College London has identified a link between the negative symptoms experienced by people with schizophrenia and adverse clinical outcomes.
Negative symptoms can include poor motivation, poor eye contact and a reduction in speech and activity. As a result, people with schizophrenia often appear emotionless, flat and apathetic. These contrast with positive symptoms - psychotic behaviours not seen in healthy people, such as delusions or hallucinations.
Published today in BMJ Open, the study is the largest- ever to investigate a relationship between negative symptoms and clinical outcomes, drawing from a sample of more than 7,500 patients.
Researchers used the Clinical Record Interactive Search (CRIS) application, a text-mining tool, to analyse anonymised patient data on negative symptoms from the South London and Maudsley NHS Foundation Trust (SLaM) Biomedical Research Centre (BRC) Case Register.
Natural Language Processing (NLP) was used to detect statements within the clinical records which determined references to specified negative symptoms. 10 negative symptoms were identified, including poor motivation, blunted or flattened mood, poor eye contact, emotional withdrawal, poor rapport, social withdrawal, poverty of speech (excessively short speech with minimal elaborations), inability to speak, apathy and concrete thinking (the inability to think in abstract terms).
They found that 41 per cent of patients showed the presence of two or more negative symptoms. Negative symptoms across the sample were associated with an increased likelihood of hospital admission, longer duration of admission and an increased likelihood of re-admission following discharge from hospital.
Patients with two or more negative symptoms were 24 per cent more likely to have been admitted to hospital. In addition, each of their admissions were, on average, an extra 21 days in duration and, when discharged, these individuals had a 58 per cent higher risk of re-admission within 12 months.
The most frequently recorded negative symptoms were poor motivation (31 per cent), blunted or flattened mood (27 per cent), poor eye contact (26 per cent) and emotional withdrawal (24 per cent).
Dr Rashmi Patel from the Department of Psychosis Studies at the IoPPN, said: "Hospital admissions are the main drivers of cost in the care of patients with schizophrenia - yet they have traditionally been linked to the severity of positive psychotic symptoms.
"Our data indicate that negative symptoms are an equally important factor, and suggest that a greater emphasis on assessing and treating these features of schizophrenia may have significant health economic benefits.
"However, as our findings are drawn from observational data, interventional clinical studies are required to determine whether an effective treatment for negative symptoms would lead to better clinical outcomes."
Journal information: BMJ Open
Provided by King's College London