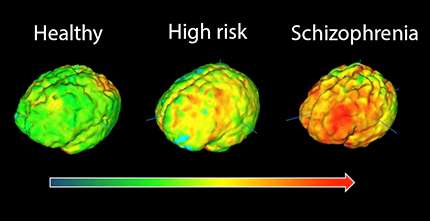
PET imaging signal in healthy volunteers, high-risk subjects and patients with schizophrenia showing elevation in immune cell inflammation as severity of illness increases. Credit: Peter Bloomfield, Sudhakar Selvaraj, Mattia Veronese and Oliver Howes.
A study published today in the American Journal of Psychiatry is the first to find that immune cells are more active in the brains of people at risk of schizophrenia as well as those already diagnosed with the disease.
The finding could completely change our current understanding of schizophrenia, raising the possibility that testing people most at risk of the disorder ahead of time could allow them to be treated early enough to avoid its most severe symptoms.
Researchers at the Medical Research Council's (MRC) Clinical Sciences Centre, based at Imperial College London, in collaboration with colleagues at the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King's College London, used positron emission tomography (PET) scans to measure levels of activity of immune cells in the brain. These cells, known as microglia, respond to damage and infection in the brain, and are also responsible for rearranging the connections between brain cells so that they work as well as possible; a process known as pruning.
The team tested a group of 56 people including those already diagnosed with schizophrenia, those at risk of the disease and those with no symptoms or risk of the disorder. They found that activity levels of microglia in the brain increased according to the severity of symptoms in people with schizophrenia and that people with diagnosed schizophrenia had high levels of activity of these immune cells in their brain.
Peter Bloomfield, lead author of the study at the MRC Clinical Sciences Centre, said: 'Our findings are particularly exciting because it was previously unknown whether these cells become active before or after onset of the disease.
'Now we have shown this early involvement, mechanisms of the disease and new medications can hopefully be uncovered.'
Dr Oliver Howes of the IoPPN at King's and head of the psychiatric imaging group at the MRC Clinical Sciences Centre, added: 'Schizophrenia is a potentially devastating disorder and we desperately need new treatments to help sufferers, and ultimately to prevent it.
'This is a promising study as it suggests that inflammation may lead to schizophrenia and other psychotic disorders. We now aim to test whether anti-inflammatory treatments can target these. This could lead to new treatments or even prevention of the disorders altogether.'
Professor Hugh Perry, Chair of the Neuroscience and Mental Health Board at the MRC, added: 'Schizophrenia, like other mental health disorders, is a complex disease that we know is caused by an interplay of genetic, behavioural and other contributing factors.
'This study adds to a growing body of research that inflammation in the brain could be one of the factors contributing to a range of disorders – including Alzheimer's, schizophrenia and depression - and with this new knowledge comes the hope of life-changing treatments.'
More information: Peter S. Bloomfield et al. Microglial Activity in People at Ultra High Risk of Psychosis and in Schizophrenia: An [ C]PBR28 PET Brain Imaging Study , American Journal of Psychiatry (2015). DOI: 10.1176/appi.ajp.2015.14101358
Journal information: American Journal of Psychiatry
Provided by King's College London