Proteomics and precision medicine
As medical professionals search for new ways to personalize diagnosis and treatment of disease, a research team at the University of Iowa has already put into practice what may be the next big step in precision medicine: personalized proteomics.
Proteomics is the large-scale analysis of all the proteins in a cell type, tissue type, or organism. In contrast to genomics, which shows how genetic differences can indicate a person's potential for developing a disease over a lifetime, proteomics takes a real-time snapshot of a patient's protein profile during the disease. Doctors can use this information to tailor diagnosis and initiate treatment, sometimes long before a conventional diagnosis even begins to home in on a cause.
"Proteomics allows us to create a precision molecular diagnosis that's totally personalized for the patient," says Vinit Mahajan, M.D., Ph.D., UI clinical assistant professor of ophthalmology and visual sciences.
Mahajan's lab recently used proteomics to devise a successful treatment strategy for a patient with uveitis, a potentially blinding eye disease that can have many causes, making it particularly difficult to diagnose and treat effectively. The team's findings are described in a paper published online Feb. 4 in the journal JAMA Ophthalmology.
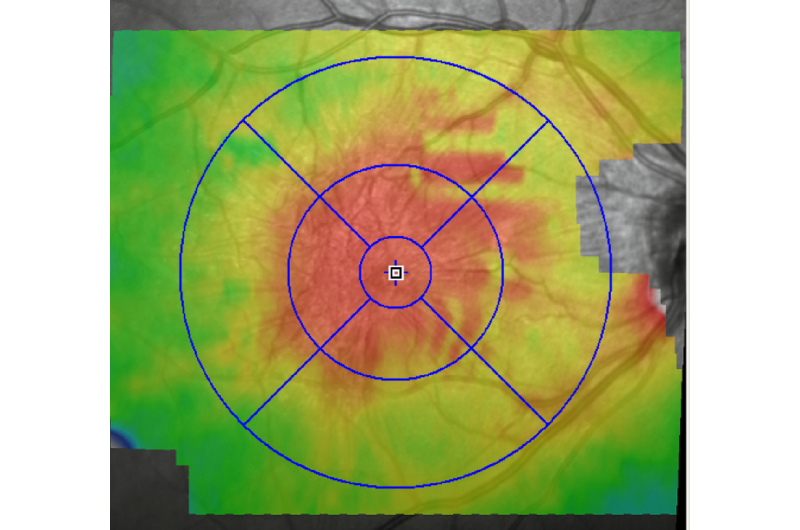
The patient had been losing vision in one eye because of relapsing inflammation and swelling in the retina, with a buildup of scar tissue. The cause was unknown, so the treatment had consisted of a trial-and-error approach based on a clinical observation of the symptoms.
"Right now, there is no precision medicine for this kind of disease," Mahajan says.
Mahajan and his team then performed a proteomic analysis of fluid taken from the patient's eye and compared that protein profile to profiles of other patients' eye fluid. Gabriel Velez, a graduate student in Mahajan's lab, spotted a pattern that closely resembled those of two other patients who were known to have an autoimmune disorder that produces antibodies against the retina.
"Her symptoms didn't look exactly like the standard clinical diagnosis for that disease," says Nathaniel Roybal, M.D., Ph.D., a vitreoretinal surgical fellow working with Mahajan. "She was missing many features. But based on this pattern that we saw, we ordered a lab test to check if she makes anti-retinal antibodies. And sure enough, the test showed that she did. So we changed how we treated her."
Mahajan performed surgery and implanted a device that continuously releases a steroid into the eye. The patient's vision improved, and she no longer has relapses.
Alexander G. Bassuk, M.D., Ph.D., associate professor in the Stead Family Department of Pediatrics at University of Iowa Children's Hospital, who co-authored the paper, says the value of personal proteomics extends beyond uveitis.
"We are using this platform to address other kinds of eye and inflammatory diseases where the best diagnosis and therapies for individual patients remain inadequate," Bassuk says.
While proteomics is being studied elsewhere, primarily for diagnostics, Mahajan says the UI implementation is unique because it uses a "whole-patient" approach that coordinates the collection, transport, storage, coding, and analysis of samples in a way that can directly and efficiently improve patient care.
"We were able to combine surgery and science and intelligently go back to the patient to decide on the optimal therapy," Mahajan says. "This is personalized precision medicine. It's the next step."
More information: Gabriel Velez et al. Precision Medicine, JAMA Ophthalmology (2016). DOI: 10.1001/jamaophthalmol.2015.5934





















