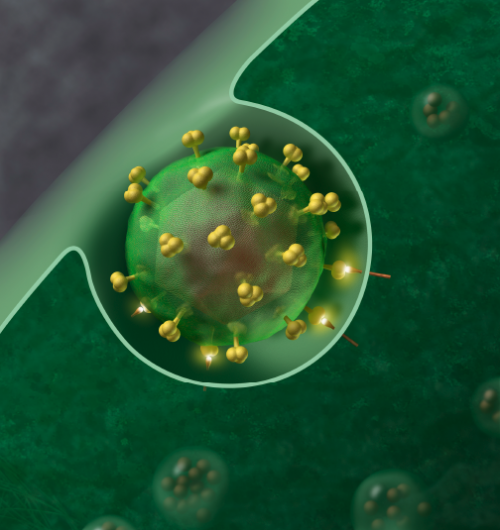
HIV-1 Virus. Credit: J Roberto Trujillo/Wikipedia
(Medical Xpress)—It's a good news/bad news scenario: Researchers have made a new discovery about HIV that will redirect curative strategies toward latent reservoirs of HIV—that's the good news. The bad news is that they discovered that clonally expanded, HIV-infected cells can can persist and produce new virus over many years in a patient on combination antiretroviral therapy (cART). Thus, any cure for HIV infection will have to attack these cells in order to permanently clear the virus.
The persistence and stubbornness of HIV infection is well documented. Since the 1980s, significant medical research has resulted in the transformation of HIV/AIDS from a terminal disease to a manageable condition. Modern antiretroviral drugs, usually used in combination, include entry inhibitors that interfere with the binding of HIV to host cells; nucleoside reverse transcriptase inhibitors that inhibit HIV integration with DNA; integrase inhibitors that block a key HIV viral enzyme; and protease inhibitors, which block a viral protease enzyme key to the maturing of virons.
However, no vaccine, drug or therapy has emerged capable of permanently curing an infected patient. Failure to adhere to a strict regimen of combination antiretroviral drugs invariably results in the recurrence of detectable HIV. One reason is the ability of latent virus to persist in cells and re-emerge in response to imperfectly understood stimuli. In the current study, published in the Proceedings of the National Academy of Sciences, a large research collaborative has established for the first time that reservoirs of infectious HIV-1 persist in CD4+ T cells that are clonally expanded–that is, a population of many cells that have been produced by a single cell. These T cell clones contain active virus that can begin to proliferate in the event of cART cessation.
It took over a decade to reach this conclusion. The results are derived from the study of a single HIV-positive patient first diagnosed with the virus in 2000. The researchers conducted virologic, immunologic, and anatomic analyses of an African-American patient from the time that he began cART until he died 13 years later from cancer. Before the publication of the study, it was unknown whether the identical viruses found in the blood cells of patients were infectious. "This result shows that cells containing replication-competent HIV-1 proviruses can clonally expand and persist in vivo, presenting a challenge for achieving a cure of HIV infection," they write.
It remains unknown which CD4 subtypes contain viable HIV (most latent reservoirs do not contain replication-competent virus), and the researchers note that further study is required to establish the mechanisms of of HIV production during persistence and clonal expansion. Nor does the present study establish whether these expansions are the result of homeostatic proliferation or a response to an antigen.
The researchers conclude, "To develop successful curative strategies, a better understanding is needed of the fraction of the replication-competent reservoir that is composed of clonally expanded cells and how to specifically target and eliminate them."
More information: Francesco R. Simonetti, et al. Clonally expanded CD4+ T cells can produce infectious HIV-1 in vivo. PNAS 2016 ; published ahead of print February 8, 2016, DOI: 10.1073/pnas.1522675113
Abstract
Reservoirs of infectious HIV-1 persist despite years of combination antiretroviral therapy and make curing HIV-1 infections a major challenge. Most of the proviral DNA resides in CD4+T cells. Some of these CD4+T cells are clonally expanded; most of the proviruses are defective. It is not known if any of the clonally expanded cells carry replication-competent proviruses. We report that a highly expanded CD4+ T-cell clone contains an intact provirus. The highly expanded clone produced infectious virus that was detected as persistent plasma viremia during cART in an HIV-1–infected patient who had squamous cell cancer. Cells containing the intact provirus were widely distributed and significantly enriched in cancer metastases. These results show that clonally expanded CD4+T cells can be a reservoir of infectious HIV-1.
Journal information: Proceedings of the National Academy of Sciences
© 2016 Medical Xpress