'Wrong' scale used to evaluate results of brain surgery
The most common scale used to evaluate outcome of neurosurgical procedures, the modified rankin scale (mRS) – does not measure what is commonly assumed, concludes a study conducted at the Department of Neurosurgery of Helsinki University Hospital. The researchers state that previous treatment results must now be reevaluated.
Surgery has become a volatile field during the past few years, with study after study challenging prevailing treatment practices. For example, surgical treatment of acute appendicitis (JAMA 2015) and arthroscopic surgery on degenerative knees (NEJM 2013) have been called into question by recent research results reached by Finnish researchers.
In neurosurgery, the evaluation of the success of treatment is challenging. Many patients undergoing surgery are either practically asymptomatic or extremely ill, meaning that the patient cannot him- or herself explain the impact of the surgery.
Consequently, the modified Rankin Scale (mRS) has been commonly used to evaluate outcome and even success of neurosurgical treatment. However, the scale was originally created to monitor the recovery process of stroke victims, not to assess the success of neurosurgery. The mRS runs from 0 to 6, and describes the patient's ability to function in broad terms, with 0 indicating no symptoms and 6 meaning that the patient is deceased. For example, a patient classified as mRS 2 exhibits slight disability, caused by whatever reason.

At least three outcome studies on cerebrovascular surgery which resulted in significant changes to neurosurgical treatment everywhere in the world used the modified Rankin Scale to compare and evaluate treatment results (Lancet 2002; Lancet 2014; Lancet 2003).
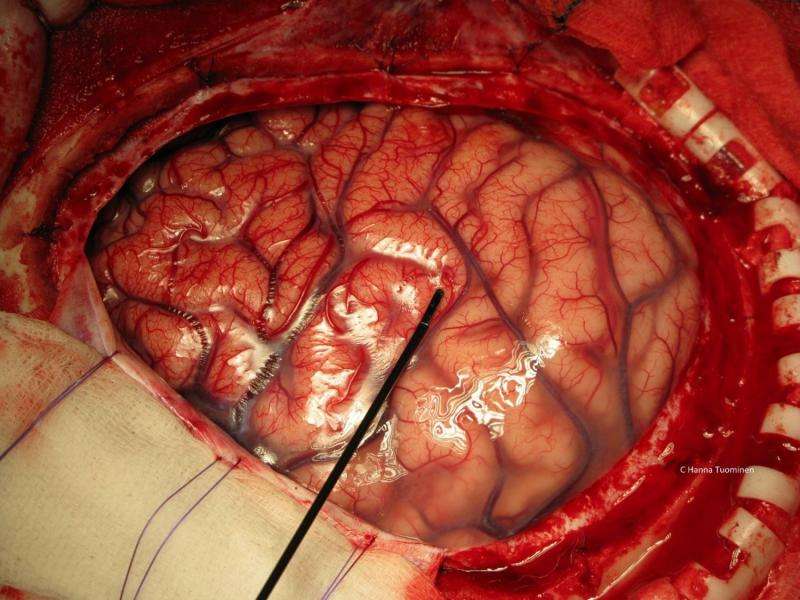
A study at the Department of Neurosurgery at the Helsinki University Hospital – one of the largest neurosurgical units in the western world – has now for the first time studied whether mRS is suitable for measuring the treatment results of brain surgery.
"We were astonished to see the results which indicate that mRS is very poorly suited to evaluating and reporting on the quality of neurosurgical treatment and related complications," says Dr. Elina Reponen, principal investigator and specialist in anaesthesiology and intensive care medicine.
According to the results, 24% of patients who underwent a normal procedure with no complications were classified with a worse mRS score 30 days after the procedure than before the surgery. This is to say that according to the mRS score, their ability to function decreased even when the treatment had been excellent and free from complications. On the other hand, 28% of patients who had experienced significant complications after surgery received an identical or better mRS score upon release. This means that the mRS score did not reflect the fact that the treatment may have been less than perfect and safe.
"The next suprise came when we found out how difficult it was to get these negative results published," Reponen says.
The non-selective follow-up study monitored patients who underwent brain surgery at the Helsinki University Hospital during one year. This means that the study is based on real patient data from a major academic neurosurgical unit.
"This is the first study examining the applicability of mRS for the assessment of neurosurgical treatment results. Based on the research, we should perhaps re-evaluate the previous studies in which the modified Rankin Scale has been used to measure treatment results and even to compare different forms of treatment. In any case, we are likely to see changes in outcomes reporting ," says Reponen.
"Neurosurgeons rarely conduct extensive research themselves, since their work is hectic and they have scant time for research. Many neurosurgical studies are led by neurologists and radiologists, who understandably choose to employ research methods and indicators which are accepted and established in their own field. However, neurosurgeons should be aware of this and consider participating in the development of the indicators used to measure their work and not outsource this task to people who are less familiar with the field," reasons neurosurgeon Miikka Korja, one of the authors of the new study.
According to Dr. Hanna Tuominen, specialist in anaesthesiology and one of the authors of the study, anaesthesiologists have been pivotal in improving and measuring patient safety in many areas of surgery, and they also have a crucial role to play in neurosurgery.
"The anaesthesiologist is on the side of both the patient and the surgeon. It is in the anaesthesiologist's interests to provide the best possible working conditions for the surgeon and the best possible outcome for the patient. This is why anaesthesiologists have been active in measuring patient safety and the quality of treatment."
More information: Elina Reponen et al. Modified Rankin Scale and short-term outcome in cranial neurosurgery -a prospective and unselected cohort study, World Neurosurgery (2016). DOI: 10.1016/j.wneu.2016.03.102
Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The appac randomized clinical trial. JAMA. 2015;313(23):2340-2348.
Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic Partial Meniscectomy versus Sham Surgery for a Degenerative Meniscal Tear. NEJM. 2013;369(26):2515-2524.
Molyneux A, Kerr R, Stratton I, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002;360(9342):1267-1274.
Mohr JP, Parides MK, Stapf C, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 2014;383:614-621.
Wiebers DO, Whishnant JP, Huston Jr, et al. Unruptured Intracranial Aneurysms: Natural History, Clinical Outcome, and Risks of Surgical and Endovascular Treatment. Lancet. 2003;362:103-110.


















