Patients with advanced lymphoma in remission after T-cell therapy
Patients with non-Hodgkin lymphoma participating in an early-phase immunotherapy trial led by Fred Hutchinson Cancer Research Center had their advanced tumors disappear completely after their immune cells were genetically engineered into cancer fighters, despite having previously exhausted multiple conventional cancer treatments, according to a new study released today. These short-term results, published today in Science Translational Medicine, are the latest from a closely watched study of these modified cells, called CAR T cells, for treating blood cancer.
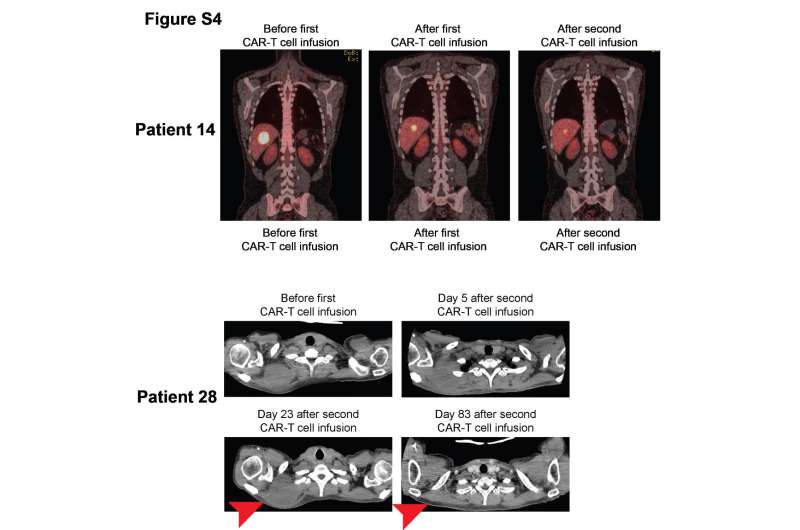
Thirty-two participants in the trial received an infusion of CAR T cells following chemotherapy (called lymphodepletion) that was given to make space in the patients' bodies for the infused CAR T cells. The team found that the CAR T cells most effectively knocked out the cancer in a group of 11 patients who received a two-drug combination chemo followed by an intermediate dose of the engineered T cells. Seven of these participants, or 64 percent, went into complete remission.
These data demonstrate how dialing in the treatment parameters can make these cells more effective cancer fighters in patients with this particular type of cancer, said Dr. Cameron Turtle, an immunotherapy researcher at Fred Hutch and one of the study leaders.
"The main message is that you can treat patients with non-Hodgkin's lymphoma with CAR T cells and get very good response rates with optimization of the CAR T-cell dose and lymphodepletion," Turtle said.
The addition of a second chemo drug in the lymphodepletion step helped the CAR T cells multiply more and survive longer in these patients than in those who had received one type of chemo, the researchers found. Among all 20 patients who received the two-drug chemo regimen, half of them achieved a complete remission, regardless of T-cell dose. (The remaining 12 patients received a different lymphodepletion regimen, and only one of them went into complete remission after CAR T-cell infusion.) "Strategies like modifying the lymphodepletion in conjunction with suitable CAR T-cell dosing can have a big impact on clinical outcome," Turtle said.
One of several ongoing trials of CAR T cells around the nation, this study's hallmark is its use of a one-to-one ratio of helper and killer CAR T cells, which join forces to kill CD19-positive tumor cells. By controlling the mixture of T cells that patients receive, the researchers can see relationships between cell doses and patient outcomes that were previously elusive.
"The idea ... is that by doing that, we would get more reproducible data around the effects of the cells—both beneficial effects against the cancer and also any side effects they might cause the patient," said Fred Hutch clinical researcher Dr. Stan Riddell, one of the senior authors on the paper, along with colleague Dr. David Maloney. "And then by adjusting the dose, we could improve what we call the therapeutic index —the benefit against the tumor—without too much toxicity."
The study team extracted disease-fighting T cells from patients' bloodstreams and sent them to a specialized lab at Fred Hutch to be re-engineered. There, technicians inserted DNA instructions for making a synthetic, cancer-targeting chimeric antigen receptor, or CAR, into the cells' genomes. The CARs used in the study, which were developed in Riddell's lab at Fred Hutch, target a molecule called CD19 that is found on the surface of certain white blood cells, including some types of lymphoma cells.
After re-engineering, the cells were multiplied in the lab using a process unique to Fred Hutch, in which cells undergo an extra growth-stimulating step. The team found that it was able to successfully generate CAR T-cell products even for patients who naturally had very few T cells. After chemo, the study team intravenously transferred the freshly engineered T cells back into the patients. There, the cells encountered their CD19 targets, began to multiply, and went to work.
"In non-Hodgkin's lymphoma, we still have very good, complete remission rates, but they're lower than those seen in acute lymphoblastic leukemia," Turtle said. "And that may relate to the fact that lymphoma often grows as lumps, so it may be a more-complex tumor microenvironment." The factors in lymphoma tumors that may impede T-cell activity—and ways to circumvent them—still need to be pinpointed, Turtle said.
More information: "Immunotherapy of non-Hodgkin's lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor-modified T cells," Science Translational Medicine, stm.sciencemag.org/lookup/doi/ … scitranslmed.aaf8621


















