Alzheimer's disease could be treated with gene therapy, animal study suggests
Researchers have prevented the development of Alzheimer's disease in mice by using a virus to deliver a specific gene into the brain.
The early-stage findings, by scientists from Imperial College London, open avenues for potential new treatments for the disease.
In the study, published in the journal Proceedings of the National Academy of Sciences, the team used a type of modified virus to deliver a gene to brain cells.
The research was funded by Alzheimer's Research UK and the European Research Council.
Previous studies by the same team suggest this gene, called PGC1 - alpha, may prevent the formation of a protein called amyloid-beta peptide in cells in the lab.
Amyloid-beta peptide is the main component of amyloid plaques, the sticky clumps of protein found in the brains of people with Alzheimer's disease. These plaques are thought to trigger the death of brain cells.
Alzheimer's disease affects around 520,000 people in the UK. Symptoms include memory loss, confusion, and change in mood or personality. Worldwide 47.5 million people are affected by dementia - of which Alzheimer's is the most common form.
There is no cure, although current drugs can help treat the symptoms of the disease.
Dr Magdalena Sastre, senior author of the research from the Department of Medicine at Imperial, hopes the new findings may one day provide a method of preventing the disease, or halting it in the early stages.
She explained: "Although these findings are very early they suggest this gene therapy may have potential therapeutic use for patients. There are many hurdles to overcome, and at the moment the only way to deliver the gene is via an injection directly into the brain. However this proof of concept study shows this approach warrants further investigation."
The modified virus used in the experiments was called a lentivirus vector, and is commonly used in gene therapy explained Professor Nicholas Mazarakis, co-author of the study from the Department of Medicine: "Scientists harness the way lentivirus infects cells to produce a modified version of the virus, that delivers genes into specific cells. It is being used in experiments to treat a range of conditions from arthritis to cancer. We have previously successfully used the lentivirus vector in clinical trials to deliver genes into the brains of Parkinson's disease patients."
In the new study, the team injected the virus, containing the gene PGC-1 - alpha, into two areas of the brain in mice susceptible to Alzheimer's disease.
The areas targeted were the hippocampus and the cortex, as these are the first regions to develop amyloid plaques in Alzheimer's disease.
Damage to the hippocampus affects short-term memory, and leads to a person forgetting recent events, such as a conversation or what they ate for breakfast. The hippocampus is also responsible for orientation, and damage results in a person becoming lost on familiar journeys, such as driving home from the shops.
The cortex, meanwhile, is responsible for long-term memory, reasoning, thinking and mood. Damage can trigger symptoms such as depression, struggling to work out how much money to give at a checkout, how to get dressed or how to cook a familiar recipe.
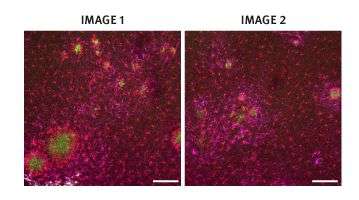
The animals were treated at the early stages of Alzheimer's disease, when they still had not developed amyloid plaques. After four months, the team found that mice who received the gene had very few amyloid plaques, compared with the untreated mice, who had multiple plaques in their brain.
Furthermore, the treated mice performed as well in memory tasks as healthy mice. The tasks included challenges such as replacing a familiar object in the mouse's cage with a new one. If the mice had a healthy memory, they would explore the new object for longer.
The team also discovered there was no loss of brain cells in the hippocampus of the mice who received the gene treatment. In addition to this, the treated mice had a reduction in the number of glial cells, which in Alzheimer's disease can release toxic inflammatory substances that cause further cell damage.
The protein PGC-1 - alpha, which is coded by the gene, is involved in metabolic processes in the body, including regulation of sugar and fat metabolism.
Dr Sastre added that other studies from different institutions suggest physical exercise and the compound resveratrol, found in red wine, may increase levels of PGC-1 - alpha protein. However, resveratrol has only been found to have benefits as a pill, rather than in wine, as the alcohol counteracts any benefit.
The team suggest injections of the gene would be most beneficial in the early stages of the disease, when the first symptoms appear.
They now hope to explore translating their findings into human treatments, said Dr Sastre. "We are still years from using this in the clinic. However, in a disease that urgently needs new options for patients, this work provides hope for future therapies."
Dr David Reynolds, Chief Scientific Officer at Alzheimer's Research UK, said: "There are currently no treatments able to halt the progression of damage in Alzheimer's, so studies like this are important for highlighting new and innovative approaches to take us towards that goal. This research sets a foundation for exploring gene therapy as a treatment strategy for Alzheimer's disease, but further studies are needed to establish whether gene therapy would be safe, effective and practical to use in people with the disease. The findings support PGC-1-alpha as a potential target for the development of new medicines, which is a promising step on the road towards developing treatments for this devastating condition."
More information: "PPARγ-coactivator-1α gene transfer reduces neuronal loss and amyloid-β generation by reducing β-secretase in an Alzheimer's disease model," by Loukia Katsouri et al. PNAS, 2016.





















