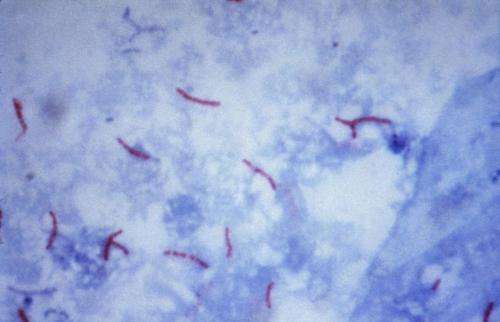
This photomicrograph reveals Mycobacterium tuberculosis bacteria using acid-fast Ziehl-Neelsen stain; Magnified 1000 X. The acid-fast stains depend on the ability of mycobacteria to retain dye when treated with mineral acid or an acid-alcohol solution such as the Ziehl-Neelsen, or the Kinyoun stains that are carbolfuchsin methods specific for M. tuberculosis. Credit: public domain
A new treatment for drug-resistant tuberculosis patients, that reported a success rate of 82 percent in a study, has been hailed as a "breakthrough" at a medical summit in Britain.
The final results were unveiled at this week's Union World Conference on Lung Health in Liverpool, north-west England, and showed patients across nine African countries responded remarkably well to the nine-month treatment.
Of the 1,006 TB sufferers who participated in the observational study of the treatment, all of whom were all resistent to TB medicine rifampicin, 734 were deemed fully cured and in a further 87 cases the treatment appeared to have worked.
Out of the remaining patients, 54 did not respond to the treatment, 49 were lost to follow-up, and 82 died.
Valerie Schwoebel, the Union's programme manager for Francophone Africa, said the treatment was chosen for scientific study because it "has emerged as a very successful combination" in the treatment of TB patients.
It was hailed as "a breakthrough in the fight against drug-resistant TB" by Paula I Fujiwara, scientific director of the International Union Against Tuberculosis and Lung Disease.
"These results have now been replicated in many different settings and with a large number of patients, showing conclusively that this is the most effective treatment for drug-resistant TB discovered to date," she said.
The Union worked alongside the Institute of Tropical Medicine in Antwerp, Belgium, the San Raffaele Scientific Institute in Milan, Italy, and local researchers to carry out the study of the treatment.
Seven drugs
Last year 1.8 million people died from tuberculosis, which is caused by a bacteria that infects the lungs, an increase of 300,000 on 2014, according to the WHO's Global TB Report 2016.
Those taking part in the newly-published study came from Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Ivory Coast, Democratic Republic of Congo, Niger and Rwanda.
During the treatment, patients were given a total of seven drugs, three of which were administered only during the first four months.
The four other drugs, one of which has previously been used to treat leprosy, were given to patients throughout the nine-month treatment.
One of those used to treat the drug-resistant TB patients, Isoniazid, was administered in a dose twice as high as that normally used to treat people infected with drug-susceptible TB.
The results come after the World Health Organization (WHO) warned earlier this month of an "uphill battle" to tackle TB globally.
"There must be a massive scale-up of efforts, or countries will continue to run behind this deadly epidemic," said Margaret Chan, WHO director general.
Last year 10.4 million people were infected with TB, up from the estimate of 9.6 million a year earlier. According to the WHO, the size of the epidemic rose largely because researchers realised that earlier estimates in India from 2000-2015 were too low.
Nearly half a million people were diagnosed with multi-drug resistant TB (MDR-TB), with about half of those cases in India, China, and the Russian Federation.
Over the past 15 years TB deaths have fallen by 22 percent, but the disease remained one of the top 10 causes of death worldwide in 2015.
© 2016 AFP