Credit: Delft University of Technology
For many patients suffering from severe obesity, a gastric sleeve (reducing the stomach) is an ideal alternative to a gastric bypass (bypassing the stomach and the first part of the intestine), which is currently the preferred solution. That is the conclusion reached by researcher and surgeon in training Pim van Rutte who has studied many aspects of this surgical intervention. On Wednesday 21 December, Van Rutte will be awarded his PhD at TU Delft for his work on the subject.
Danger
"Obesity is one of the biggest risks to public health in the 21st century. For most patients with a chronic weight problem (morbid obesity), surgery is the only treatment guaranteed to be effective in the long term," says Pim van Rutte, surgeon in training and doctoral candidate at TU Delft.
"There is as yet no clear agreement regarding which surgical technique is best suited to which patient. This is partly due to the lack of knowledge about the exact working mechanisms of this type of surgery. The original idea (to force a patient to eat less and so limit food consumption) appears to be less important, and attention is now focusing on metabolic and hormonal changes and changes to intestinal bacteria. Moreover, no long-term results are yet available on which to base a definitive statement about the effectiveness of the treatment."
Sleeve
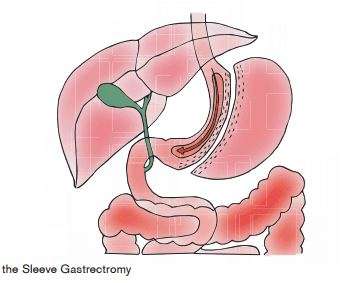
"A gastric bypass, which involves bypassing the stomach and the first part of the intestine, is still considered the gold standard," Van Rutte explains. "But the results of gastric sleeve surgery are similar to this gold standard. This method involves removing eighty per cent of the stomach's capacity. Unlike the bypass operation, the small intestine and the stomach sphincter remain untouched. This treatment has fewer long-term complications.
Gastric sleeves are being employed increasingly around the world. However, before gastric sleeve surgery can be recognised and acknowledged as the preferred treatment for morbid obesity it is necessary to examine the advantages and disadvantages of the procedure critically," says Van Rutte.
Weight loss
Van Rutte has studied gastric sleeve surgery extensively together with Catharina Hospital in Eindhoven. Only two other studies have been published describing the results of over a thousand sleeve gastrectomies. And these speak volumes. "It appears to be possible to reduce the patients overweight by at least two-thirds after two years. Maximum weight loss was achieved after four years. Moreover, many of the conditions closely associated with obesity disappear, such as diabetes and hypertension. Of the patients who had diabetes, sixty per cent experienced full remission after one year (a result comparable to gastric bypass surgery).
Van Rutte also examined the more technical aspects of the surgical procedure in order to develop a standardised and reproducible operation. Sixty interventions were filmed and systematically assessed by two independent researchers according to the Observation Clinical Human Reliability Assessment standard. A group of experts established thirteen key stages for gastric sleeve surgery and each stage was assessed and examined for mistakes with or without consequences. The average length of the procedure was reduced significantly in the period of the study to 41 minutes and this also applies to the percentage of complications, although the technique remained more or less consistent.
Stapling
Stapling the stomach turned out to be a crucial step in the procedure. "If this step is performed inadequately it can cause serious complications. Excessive or insufficient staple pressure on the stomach can result in a leak in the staple line. We found that staple line leaks occurred in 2.3 per cent of patients; 2.6 per cent suffered postoperative bleeding."
"What we need is a device to measure the thickness of the stomach wall before surgery and to advise immediately on what size staples to use."
Gold standard
"Gastric sleeves have the potential to become the new gold standard for morbid obesity, including for elderly patients, and especially for patients who are not specifically recommended for a gastric bypass," Van Rutte concludes. "The treatment should be seen as part of a process comprising three successive phases: pre-operative screening, the operation and postoperative follow-up. In recent years and working jointly with TU Delft and other institutions, adjustments have been made to each of these phases to create a standardised, reproducible and learnable process focusing especially on safety and efficiency."
"A vital aspect is careful patient selection following meticulous screening while special attention must be paid to reducing the main complications, such as leakage from the staple line and postoperative haemorrhage. After surgery, the focus should shift to a proper postoperative support. Those who suffer from morbid obesity will always will always be a patient, so that a lifelong effort is required and change of lifestyle is essential. Patients need five years of psychological, nutritional and physiotherapeutic support and outpatient follow-up."
More information: Rutte's dissertation is available online: repository.tudelft.nl/islandora/object/uuid%3A91549107-7a2e-470c-8e08-cc3aa7200f42?collection=research
Provided by Delft University of Technology